Venereal disease: Difference between revisions
imported>Nancy Sculerati |
mNo edit summary |
||
| (46 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
[[Image:278px-Mugwump Specific.png|thumb|left | {{subpages}} | ||
'''Venereal diseases''' are | {{TOC|right}} | ||
[[Image:278px-Mugwump Specific.png|thumb|left|Before [[antibiotics]] were invented, infections of [[syphilis]] and [[gonorrhea]] were common, but effective treatments were rare. The medications that actually had an effect on the disease were also toxic to the patient, [[heavy metal]] compounds being the best of them. Patent medicines were widely available in the USA in the 19th century - whether they worked or not.]] | |||
'''Venereal diseases''' are [[infection]]s spread through sexual contact. What is special about such diseases is the germs that cause them- these agents, whether they be bacteria, viruses, or other types of microorganisms, can only remain infectious if kept at the conditions that exist inside a living person. Unlike the virus that causes the common cold, once they leave the body's warm environment, with its supplies of oxygen and nutrients and living cells, they cannot survive. The pathogens that cause venereal disease can infect solely by passing directly from one body into another, through living fluids. When the term, "venereal disease" was coined, in the 19th century, sexual activity was the ''only'' prolonged "intimate" means of sharing body fluids that occurred with any regularity, except for the special case of mother and infant during pregnancy and at birth. Since that time, with the advent of blood transfusion, organ transplant, and groups of substance abusers who share hypodermic equipment for injecting drugs, some of the same fastidious organisms that could only survive transmission from an infected person to a new host through sexual contact now are also able to survive through these other forms of transport. <ref>{{citation | |||
| author = Gerbase AC, Rowley JT, Mertens TE | |||
| title=Global epidemiology of sexually transmitted diseases | |||
| journal = Lancet | |||
| year = 1998 | |||
| volume= 351 (suppl III) | |||
| pages =2–4 | |||
}}</ref> | |||
Some venereal diseases can be passed from an infected mother to her baby: either during pregnancy, birth, or through breastfeeding. This fact has changed the utility of breastfeeding in some areas, like sub-Saharan Africa, where the rate of HIV (which is transmitted in breast milk) is very high. It also had an influence on the social mores of Europe, where, after syphilis became epidemic in the 15th century, women warned their daughters about the dangers of marrying the wrong man, lest the children bring tragedy. | Some venereal diseases can be passed from an infected mother to her baby: either during pregnancy, birth, or through breastfeeding. This fact has changed the utility of breastfeeding in some areas, like sub-Saharan Africa, where the rate of HIV (which is transmitted in breast milk) is very high. It also had an influence on the social mores of Europe, where, after [[syphilis]] became epidemic in the 15th century, women warned their daughters about the dangers of marrying the wrong man, lest the children bring tragedy. | ||
[[Sexually transmitted disease]]s (STD) include ''both'' the venereal diseases and other infections. These other kinds of infections can be spread in ''many'' ways, but are so likely to be transmitted by sexual contact with an infected person that they are included in the category. | [[Sexually transmitted disease]]s (STD) include ''both'' the venereal diseases and other infections. These other kinds of infections can be spread in ''many'' ways, but are so likely to be transmitted by sexual contact with an infected person that they are included in the category. | ||
Public health and infectious disease experts relate the incidence of venereal diseases to several factors. The first is the rate of spread, in venereal diseases that is related both to the number of infected people, how often susceptible people have sex with those who are infected, and how frequently each infected person has sex with new contacts. The second is how long the infected people remain both infected and sexually active, the longer that duration, the greater the spread. The third is how efficiently the disease is spread with each exposure to a susceptible person. Although [[Contraception (medical methods)|male condoms]] can markedly decrease the efficiency of spread of these diseases, they do not prevent spread altogether. Some of the diseases, like chancroid or herpes, that cause open "wounds" on the genitals, increase the chances of catching other venereal diseases from an infected partner, notably HIV. HIV, by decreasing immune response, lowers the resistance to the HIV infected person to most infections, and notably to certain of the venereal diseases, like [[syphilis]]. For example, co-infection with HIV increases syphilis' severity, and, in particular, increases the likelihood that [[syphilis]] will affect the [[brain]] and [[central nervous system]] | |||
==Venereal disease of bacterial origin== | ==Venereal disease of bacterial origin== | ||
===Syphilis=== | ===Syphilis=== | ||
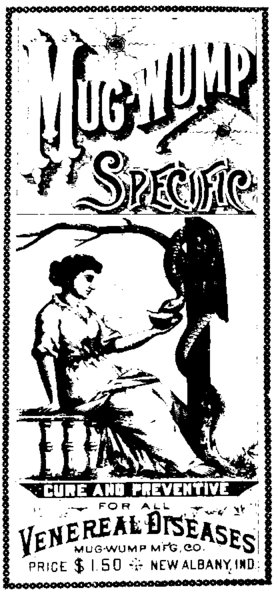
[[Image:TreponemaPallidum.jpg||thumb|right|150 px|An electron micrograph of the spirochete, [[Treponema | [[Image:TreponemaPallidum.jpg||thumb|right|150 px|An electron micrograph of the spirochete, [[Treponema pallidum]], that causes [[syphilis]].]] | ||
"Worldwide, there are an estimated 12 million new syphilis cases every year, over 90% of which occur in developing countries."(reference for quote:Gaudio PA. Update on ocular syphilis. Current Opinion in Ophthalmology. 17(6):562-6, 2006 Dec. UI: 17065926) | {{main|Syphilis}} | ||
"Worldwide, there are an estimated 12 million new [[syphilis]] cases every year, over 90% of which occur in developing countries."(reference for quote:Gaudio PA. Update on ocular syphilis. Current Opinion in Ophthalmology. 17(6):562-6, 2006 Dec. UI: 17065926). Since early syphilis is now curable with medical treatment, persistent cases are the result of either (1) the lack of available medical care (which accounts for the predominance of cases in the developing world), (2) medical negligence or misdiagnosis, or (3) the failure of the infected individual to seek medical attention or to complete recommended treatment. That failure generally occurs either because the individual does not understand that he or she may have an infection that requires treatment, or because of apathy towards self-care. | |||
== | ===Gonorrhea=== | ||
{{main|Gonorrhea}} | |||
When men and women are newly infected with gonorrhea, the symptoms depend on the route of entry. For both men and women the genital tract is usually infected. In men, there is usually a discharge from the penis. In women, the infection in the early stages is rarely has any signs or symptoms. Despite that, it is women who more commonly have the more serious problems from gonorrhea. That's because she is unlikely to seek treatment unless informed of the risk of disease by the man who infected her, and, without antibiotic treatment, the bacteria will often go on to infect the upper reproductive tract, causing inflammation and scarring of the fallopian tubes (salpingitis) and go on to cause infertility. | |||
====Gonorrhea in historical perspective==== | |||
"The history of sexually transmitted diseases is thought to date back to earliest times, and many ancient texts describe conditions that may be those of syphilis and gonorrhea, which at one time were thought to be the same disease."<ref>:{{citation | |||
| author = Ligon BL | |||
| title = Albert Ludwig Sigesmund Neisser: discoverer of the cause of gonorrhea. | |||
| journal = Seminars in Pediatric Infectious Diseases | |||
| volume = 16 | |||
| issue = 4 | |||
| pages = 336-41 | |||
| date = 2005 Oct}}</ref> Ulcers on the genitals that appeared on men and women after sexual intercourse are described in Egyptian papyri. "A 12th century commentator, Rabbi Shlomo Yitzhati, wrote that the Hebrew word "Zav" ("issue") described a discharge the colour of "rice water". Celsus (25 BC--50 AD) described profusio seminis as the shedding of semen which occurs without sexual desire or erotic dreams, and in such a way that in time, the patient is consumed by wasting. [4] Galen (130-200 AD) originated the word gonorrhoea (Greek gonos, semen, and rhoia, to flow). He defined it as "an unwanted secretion of semen without erection.""<ref>{{citation | |||
| author = Oriel JD | |||
| title = The history of non-gonococcal urethritis | |||
| journal = Genitourinary Medicine | |||
| volume = 72( | |||
| issue = 5 | |||
| pages = 374-9 | |||
| date=1996 Oct. UI}}</ref> | |||
After the epidemic of syphilis began in the 15th and 16th centuries, some [[physician]]s thought that it was the same illness as gonorrhea, but by the 18th century, it was accepted that there was a distinction in the two diseases. Certainly, we know that some patients are infected with both, and that must have added to the confusion over diagnosis. | |||
The organism that causes Gonorrhea is also a bacteria, but unlike the spirochete that causes syphilis, this is a bacteria that is of a much more common shape and kind in terms of human infection, and that has remained much more sensitive to complete eradication by antibiotics throughout all stages of infection. None the less, although gonorrhea is generally a much more limited disease than syphilis, it can cause lesions in multiple organs and, in women, is associated with pelvic inflammatory disease. | |||
The infecting organism is the diplococcus bacteria Neisseria gonorrhoeae, which is negative on [[Gram stain]]."The introduction of treatment for gonorrhea also resulted in a decline in incidence during the 1950s, but, unlike syphilis, periodic oscillations did not ensue". | |||
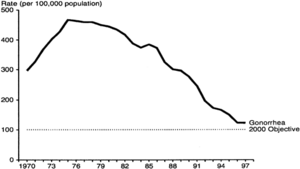
[[Image:SA7-SB3-SC27-SD1-C280-FF1.gif.png|thumb|left|300 px|Rates of gonorrhea reported to the United States CDC1970–1997. A peak of approximately 500 reported cases per 100,000 population in 1975 fell to below 125 cases per 100,000 population in 1996. The presumed cause of this decline is greater use of condoms and caution about venereal disease in the wake of the AIDS crisi. (From Division of STD Prevention. Sexually Transmitted Disease Surveillance, 1997. U.S. Department of Health and Human Services. Atlanta: Centers for Disease Control and Prevention, September 1998;)]] | |||
for | |||
"There is no known protective immunity for uncomplicated gonococcal infection; a person can have repeated infections. The highly variable surface antigens help gonococci to evade antibodies and repeatedly infect humans."<ref> Chapter 280- GONOCOCCAL INFECTIONS ''in'' H. David Humes, Herbert L. DuPont et al (Eds) :Kelley's textbook of internal medicine.—4th ed.ISBN 0781717876</ref> | |||
====Disseminated gonorrhea==== | |||
====Congenital gonorrhea==== | |||
[[Image: | [[Image:Gonococcal ophthalmia neonatorum.jpg|thumb|right|300 px|This young infant was born to a mother infected with gonorrhea and developed this bacterial infection of both eyes (''gonococcal ophthalmia neonatorum)''. It was completely cured with antibiotics.]] | ||
When infants are born to mothers with gonorrhea infections of the [[cervix]] and birth canal, their fate is highly dependant upon the medical treatment that is received. In many hospitals, there is a routine placement of dilute silver nitrate drops in the eyes of all newborns. This measure has been very effective in preventing the most common problem that such babies develop, a bacterial [[conjunctivitis]] that can cause blindness if no medical care is available for the baby.Less commonly, infants may have skin abscesses, vaginal infections, and arthritis from gonorhea contracted from their mother during birth. There are more serious problems that babies who are delivered through a birth canal infected with N. gonorrhea face however, and that is a disseminated gonorrheal infection. Although this infection, which occurs when the bacteria enter the baby's bloodstream, may be fatal without treatment, with aggressive intravenous antibiotic treatment the baby may recover completely. | |||
Gonorrhea infections have a very different impact on babies in the developed world than on those infants born to mothers in parts of the world where medical attention and antibiotic treatment are not generally available. In the developing world, permanent disability and death are not uncommon when a neonate contracts gonorrhea at birth.<ref>{{citation | |||
| author = Erdem G. Schleiss MR | |||
| title = Gonococcal bacteremia in a neonate | |||
| journal = Clinical Pediatrics | |||
|volume = 39 | |||
| issue = 1 | |||
|pages = 43-4 | |||
| date = 2000 Jan}}</ref> | |||
=== | ===Chancroid === | ||
[[Image:Haemophilus ducreyi 5811 lores.jpg|thumb|right|Buboes: greatly enlarged inguinal lymph nodes, the skin is discolored over them, rupture is likely to occur.]] | |||
[[Chancroid]] is a venereal disease most common in Africa, and the developing world. Caused by the bacteria ''Hemophilius ducreyi'', the hallmark of this disease is giant genital ulcers. Although some women are colonized by the bacteria without developing lesions, others do develop ulcers. It is men, however-particularly uncircumcised men, that bear the bulk of the lesions of this disease.Since women may be infected and harbor the bacteria without obvious disease, it is asymptomatic infected women who are primary carriers. About half of the men and women with ulcers also have enlarged lymph nodes in the groin (inguinal lymphadenopathy). The tissue in the center of these lymph glands often dies, becoming necrotic, and the mass in the groin then becomes soft and fluctuant. Rupture of these masses with spontaneous drainage may occur. Greatly enlarged lymph nodes with spontaneous rupture in this manner are sometimes called buboes, and are also a mark of plague. | |||
Many people have called AIDS a modern plague, and chancroid is particularly harmful in areas where HIV, the human immunodeficiency virus that causes AIDS, is prevalent . The patent with chancroid is at higher risk for HIV infection because the open ulcers offer a wide portal of entry. These open ulcers in men are one route of female-male HIV infection that helps account for the equal incidence of AIDS seen in men and women in Africa. | |||
===Lymphogranuloma Venereum=== | |||
Caused by ''Chlamydia trachomatis'', the disease (LGV) is rare in North America, most of Asia, and Australia, but | |||
endemic in East and West Africa, India, Southeast Asia, South America, and the Caribbean. Its incidence in Europe has increased since 2003. The disease is primarily sexually transmitted, but transmission through aerosols, nonsexual personal contact, and accidental laboratory exposures. It has also been transmitted through oral sex. <ref name=Bushnell2007>{{citation | |||
| date = 2 October 2007 | |||
| title = Lymphogranuloma Venereum | |||
| journal = eMedicine | |||
| url = http://www.emedicine.com/emerg/TOPIC304.HTM | |||
| first = Andrew C | last =Bushnell}}</ref> | |||
It is a disease of the [[lymph node]]s, traveling from the point of entry via the [[lymphatic]]s, and occurs in three stages. Frequently, it is unrecognized until the third stage. | |||
*Primary: painless herpetiform ulcer at the point of entry | |||
*Secondary: painful lymph nodes | |||
*Tertiary: years after the first infection, this is most often found in women and in homosexual men, as abscesses, fistulae, and strictures of the vagina or rectum. | |||
===Ureaplasma and mycoplasma=== | |||
''Ureaplasma'' and ''Mycoplasma'' species, the simplest of free-living organisms, which lack a cell wall, still can produce localized urogenital disease. They can also produce localized urogenital diseases. They may be present in asymptomatic patients, but manifest when the host is immunosuppressed. They may manifest in a great number of ways, including urethritis. Since they are not detectable by normal laboratory tests, this may be more of a disease of exclusion. Septic arthritis may be a clue.<ref name=>{{citation | |||
| url = http://www.emedicine.com/med/TOPIC2340.HTM | |||
| title = Ureaplasma infections | |||
| first = Ken B | last =Waite | |||
| journal = eMedicine | |||
| date = 27 March 2008}}</ref> | |||
They are not covered by the most common antibiotics. [[Doxycycline]] had been the drug of choice, but resistance has developed; local clinical experience should guide the choice of antibiotics. Macrolides (e.g., [[azithromycin]]) and fluoroquinolones (e.g., [[ciprofloxacin]]) may be effective if [[tetracycline]]s do not work. | |||
[[ | |||
==Venereal disease of viral origin== | ==Venereal disease of viral origin== | ||
The venereal diseases listed here are caused by the transmission of viruses. Even so, the symptoms that they cause, in some cases, may be mistaken for venereal diseases spread by bacteria and for other illnesses, that are non-venereal in nature. | The venereal diseases listed here are caused by the transmission of viruses. Even so, the symptoms that they cause, in some cases, may be mistaken for venereal diseases spread by bacteria and for other illnesses, that are non-venereal in nature. | ||
===Herpes simplex=== | ===Herpes simplex=== | ||
Genital [[herpes]], syphilis, and chancroid are the most prevalent causes of genital ulcers. Genital herpes, unlike syphilis or chancroid, is caused by a virus and therefore, like all viruses, is not treatable with antibiotics. At this time, although there are anti-viral treatments for the Herpes simplex viruses that cause genital herpes;there is no cure. Once contracted, herpes is a lifelong disease characterized by recurrent outbreaks. | {{main|Herpes simplex virus}} | ||
[[Image:HerpesCDC.jpg|thumb|left|300 px| A single vesicle of Herpes simplex shown in close-up on the penile glans. This particular lesion was found to be due to HSV 2, but the vesicles of both Herpes 1 and Herpes 2 look just the same. This is the "drop of water on a rose petal" appearance of the early vesicle, before there is surrounding swelling and before the vesicular rash begins to crust. | |||
]]Genital [[herpes simplex virus]], syphilis, and chancroid are the most prevalent causes of genital ulcers. Genital herpes, unlike syphilis or chancroid, is caused by a virus and therefore, like all viruses, is not treatable with antibiotics. At this time, although there are anti-viral treatments for the Herpes simplex viruses that cause genital herpes;there is no cure. Once contracted, herpes is a lifelong disease characterized by recurrent outbreaks. | |||
===Human papillomavirus (HPV)=== | ===Human papillomavirus (HPV)=== | ||
{{main|Human papilloma virus (HPV)}} | |||
[[Human papilloma virus (HPV)]] is a viral wart that includes strains spread by sexual contact. Like some other venereal diseases, these strains can also be contracted by infants from their mothers. Certain types of the sexually transmitted virus have a high rate of malignant transformation of infected cells. The cells that the virus infects are epthelial cells, either skin cells or mucosa cells, and the transformation is to squamous cell carcinoma. The potential for a viral strain to cause malignant transformation is called " oncogenic potential". This oncogenic effect is most common in women with cervical infections, and is the single major cause of cervical [[cancer]], but it also occurs in anal lesions in both men and women, causing anal squamous cell carcinoma, and squamous cell carcinoma of the lung, larynx and bronchi in children with [[congenital laryngeal papillomatosis]]. | |||
"More than 100 HPV types are recognized, and individual types are associated with specific clinical manifestations. For example, HPV-1 causes plantar warts, HPV-6 causes anogenital warts, and HPV-16 infection can produce cervical dysplasia and invasive cervical cancer." <ref>{{citation | |||
| first = Richard C. | last = Reichman | |||
| chapter = Chapter 169. Human Papillomavirus Infections | |||
| title = Harrison's Principles of Internal Medicine, 16th Edition}}</ref> "At least 30 HPV types infect the genital area, of which 15 are classified as high risk, that is, having oncogenic potential"<ref name=Barnabas>{{citation | |||
| author = Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, et al. | |||
| titme = Epidemiology of HPV 16 and Cervical Cancer in Finland and the Potential Impact of Vaccination: Mathematical Modelling Analyses | |||
journal = PLoS Medicine | |||
| volume = 3 | |||
| issue =5 | |||
| page = 138 | |||
| doi=10.1371/journal.pmed.0030138}}</ref> | |||
Recent studies have suggested that condoms are ''not'' highly effective in preventing HPV infection. | |||
====Cervical cancer==== | |||
{{main|Cervical cancer}} | |||
Epidemiologic studies combined with mathematical modelling indicate that universal vaccination of young women is likely to markedly decrease the incidence of cervical cancer.<ref name=Barnabas /> | |||
===HIV=== | ===HIV=== | ||
{{main|Human Immunodeficiency Virus}} | |||
Unlike the other venereal diseases discussed here, human immunodeficiency viruses does not affect the appearance of the genitals or other entry site into the body. Instead, there is a systemic infection that lodges in a certain type of white blood cell, the lymphocyte, of the new host. | |||
==References== | ==References== | ||
{{reflist|2}} | |||
[[Category:Suggestion Bot Tag]] | |||
[[Category: | |||
Latest revision as of 17:00, 4 November 2024
Venereal diseases are infections spread through sexual contact. What is special about such diseases is the germs that cause them- these agents, whether they be bacteria, viruses, or other types of microorganisms, can only remain infectious if kept at the conditions that exist inside a living person. Unlike the virus that causes the common cold, once they leave the body's warm environment, with its supplies of oxygen and nutrients and living cells, they cannot survive. The pathogens that cause venereal disease can infect solely by passing directly from one body into another, through living fluids. When the term, "venereal disease" was coined, in the 19th century, sexual activity was the only prolonged "intimate" means of sharing body fluids that occurred with any regularity, except for the special case of mother and infant during pregnancy and at birth. Since that time, with the advent of blood transfusion, organ transplant, and groups of substance abusers who share hypodermic equipment for injecting drugs, some of the same fastidious organisms that could only survive transmission from an infected person to a new host through sexual contact now are also able to survive through these other forms of transport. [1]
Some venereal diseases can be passed from an infected mother to her baby: either during pregnancy, birth, or through breastfeeding. This fact has changed the utility of breastfeeding in some areas, like sub-Saharan Africa, where the rate of HIV (which is transmitted in breast milk) is very high. It also had an influence on the social mores of Europe, where, after syphilis became epidemic in the 15th century, women warned their daughters about the dangers of marrying the wrong man, lest the children bring tragedy.
Sexually transmitted diseases (STD) include both the venereal diseases and other infections. These other kinds of infections can be spread in many ways, but are so likely to be transmitted by sexual contact with an infected person that they are included in the category.
Public health and infectious disease experts relate the incidence of venereal diseases to several factors. The first is the rate of spread, in venereal diseases that is related both to the number of infected people, how often susceptible people have sex with those who are infected, and how frequently each infected person has sex with new contacts. The second is how long the infected people remain both infected and sexually active, the longer that duration, the greater the spread. The third is how efficiently the disease is spread with each exposure to a susceptible person. Although male condoms can markedly decrease the efficiency of spread of these diseases, they do not prevent spread altogether. Some of the diseases, like chancroid or herpes, that cause open "wounds" on the genitals, increase the chances of catching other venereal diseases from an infected partner, notably HIV. HIV, by decreasing immune response, lowers the resistance to the HIV infected person to most infections, and notably to certain of the venereal diseases, like syphilis. For example, co-infection with HIV increases syphilis' severity, and, in particular, increases the likelihood that syphilis will affect the brain and central nervous system
Venereal disease of bacterial origin
Syphilis
"Worldwide, there are an estimated 12 million new syphilis cases every year, over 90% of which occur in developing countries."(reference for quote:Gaudio PA. Update on ocular syphilis. Current Opinion in Ophthalmology. 17(6):562-6, 2006 Dec. UI: 17065926). Since early syphilis is now curable with medical treatment, persistent cases are the result of either (1) the lack of available medical care (which accounts for the predominance of cases in the developing world), (2) medical negligence or misdiagnosis, or (3) the failure of the infected individual to seek medical attention or to complete recommended treatment. That failure generally occurs either because the individual does not understand that he or she may have an infection that requires treatment, or because of apathy towards self-care.
Gonorrhea
When men and women are newly infected with gonorrhea, the symptoms depend on the route of entry. For both men and women the genital tract is usually infected. In men, there is usually a discharge from the penis. In women, the infection in the early stages is rarely has any signs or symptoms. Despite that, it is women who more commonly have the more serious problems from gonorrhea. That's because she is unlikely to seek treatment unless informed of the risk of disease by the man who infected her, and, without antibiotic treatment, the bacteria will often go on to infect the upper reproductive tract, causing inflammation and scarring of the fallopian tubes (salpingitis) and go on to cause infertility.
Gonorrhea in historical perspective
"The history of sexually transmitted diseases is thought to date back to earliest times, and many ancient texts describe conditions that may be those of syphilis and gonorrhea, which at one time were thought to be the same disease."[2] Ulcers on the genitals that appeared on men and women after sexual intercourse are described in Egyptian papyri. "A 12th century commentator, Rabbi Shlomo Yitzhati, wrote that the Hebrew word "Zav" ("issue") described a discharge the colour of "rice water". Celsus (25 BC--50 AD) described profusio seminis as the shedding of semen which occurs without sexual desire or erotic dreams, and in such a way that in time, the patient is consumed by wasting. [4] Galen (130-200 AD) originated the word gonorrhoea (Greek gonos, semen, and rhoia, to flow). He defined it as "an unwanted secretion of semen without erection.""[3]
After the epidemic of syphilis began in the 15th and 16th centuries, some physicians thought that it was the same illness as gonorrhea, but by the 18th century, it was accepted that there was a distinction in the two diseases. Certainly, we know that some patients are infected with both, and that must have added to the confusion over diagnosis.
The organism that causes Gonorrhea is also a bacteria, but unlike the spirochete that causes syphilis, this is a bacteria that is of a much more common shape and kind in terms of human infection, and that has remained much more sensitive to complete eradication by antibiotics throughout all stages of infection. None the less, although gonorrhea is generally a much more limited disease than syphilis, it can cause lesions in multiple organs and, in women, is associated with pelvic inflammatory disease.
The infecting organism is the diplococcus bacteria Neisseria gonorrhoeae, which is negative on Gram stain."The introduction of treatment for gonorrhea also resulted in a decline in incidence during the 1950s, but, unlike syphilis, periodic oscillations did not ensue".
"There is no known protective immunity for uncomplicated gonococcal infection; a person can have repeated infections. The highly variable surface antigens help gonococci to evade antibodies and repeatedly infect humans."[4]
Disseminated gonorrhea
Congenital gonorrhea
When infants are born to mothers with gonorrhea infections of the cervix and birth canal, their fate is highly dependant upon the medical treatment that is received. In many hospitals, there is a routine placement of dilute silver nitrate drops in the eyes of all newborns. This measure has been very effective in preventing the most common problem that such babies develop, a bacterial conjunctivitis that can cause blindness if no medical care is available for the baby.Less commonly, infants may have skin abscesses, vaginal infections, and arthritis from gonorhea contracted from their mother during birth. There are more serious problems that babies who are delivered through a birth canal infected with N. gonorrhea face however, and that is a disseminated gonorrheal infection. Although this infection, which occurs when the bacteria enter the baby's bloodstream, may be fatal without treatment, with aggressive intravenous antibiotic treatment the baby may recover completely.
Gonorrhea infections have a very different impact on babies in the developed world than on those infants born to mothers in parts of the world where medical attention and antibiotic treatment are not generally available. In the developing world, permanent disability and death are not uncommon when a neonate contracts gonorrhea at birth.[5]
Chancroid
Chancroid is a venereal disease most common in Africa, and the developing world. Caused by the bacteria Hemophilius ducreyi, the hallmark of this disease is giant genital ulcers. Although some women are colonized by the bacteria without developing lesions, others do develop ulcers. It is men, however-particularly uncircumcised men, that bear the bulk of the lesions of this disease.Since women may be infected and harbor the bacteria without obvious disease, it is asymptomatic infected women who are primary carriers. About half of the men and women with ulcers also have enlarged lymph nodes in the groin (inguinal lymphadenopathy). The tissue in the center of these lymph glands often dies, becoming necrotic, and the mass in the groin then becomes soft and fluctuant. Rupture of these masses with spontaneous drainage may occur. Greatly enlarged lymph nodes with spontaneous rupture in this manner are sometimes called buboes, and are also a mark of plague.
Many people have called AIDS a modern plague, and chancroid is particularly harmful in areas where HIV, the human immunodeficiency virus that causes AIDS, is prevalent . The patent with chancroid is at higher risk for HIV infection because the open ulcers offer a wide portal of entry. These open ulcers in men are one route of female-male HIV infection that helps account for the equal incidence of AIDS seen in men and women in Africa.
Lymphogranuloma Venereum
Caused by Chlamydia trachomatis, the disease (LGV) is rare in North America, most of Asia, and Australia, but endemic in East and West Africa, India, Southeast Asia, South America, and the Caribbean. Its incidence in Europe has increased since 2003. The disease is primarily sexually transmitted, but transmission through aerosols, nonsexual personal contact, and accidental laboratory exposures. It has also been transmitted through oral sex. [6]
It is a disease of the lymph nodes, traveling from the point of entry via the lymphatics, and occurs in three stages. Frequently, it is unrecognized until the third stage.
- Primary: painless herpetiform ulcer at the point of entry
- Secondary: painful lymph nodes
- Tertiary: years after the first infection, this is most often found in women and in homosexual men, as abscesses, fistulae, and strictures of the vagina or rectum.
Ureaplasma and mycoplasma
Ureaplasma and Mycoplasma species, the simplest of free-living organisms, which lack a cell wall, still can produce localized urogenital disease. They can also produce localized urogenital diseases. They may be present in asymptomatic patients, but manifest when the host is immunosuppressed. They may manifest in a great number of ways, including urethritis. Since they are not detectable by normal laboratory tests, this may be more of a disease of exclusion. Septic arthritis may be a clue.[7]
They are not covered by the most common antibiotics. Doxycycline had been the drug of choice, but resistance has developed; local clinical experience should guide the choice of antibiotics. Macrolides (e.g., azithromycin) and fluoroquinolones (e.g., ciprofloxacin) may be effective if tetracyclines do not work.
Venereal disease of viral origin
The venereal diseases listed here are caused by the transmission of viruses. Even so, the symptoms that they cause, in some cases, may be mistaken for venereal diseases spread by bacteria and for other illnesses, that are non-venereal in nature.
Herpes simplex

Genital herpes simplex virus, syphilis, and chancroid are the most prevalent causes of genital ulcers. Genital herpes, unlike syphilis or chancroid, is caused by a virus and therefore, like all viruses, is not treatable with antibiotics. At this time, although there are anti-viral treatments for the Herpes simplex viruses that cause genital herpes;there is no cure. Once contracted, herpes is a lifelong disease characterized by recurrent outbreaks.
Human papillomavirus (HPV)
Human papilloma virus (HPV) is a viral wart that includes strains spread by sexual contact. Like some other venereal diseases, these strains can also be contracted by infants from their mothers. Certain types of the sexually transmitted virus have a high rate of malignant transformation of infected cells. The cells that the virus infects are epthelial cells, either skin cells or mucosa cells, and the transformation is to squamous cell carcinoma. The potential for a viral strain to cause malignant transformation is called " oncogenic potential". This oncogenic effect is most common in women with cervical infections, and is the single major cause of cervical cancer, but it also occurs in anal lesions in both men and women, causing anal squamous cell carcinoma, and squamous cell carcinoma of the lung, larynx and bronchi in children with congenital laryngeal papillomatosis.
"More than 100 HPV types are recognized, and individual types are associated with specific clinical manifestations. For example, HPV-1 causes plantar warts, HPV-6 causes anogenital warts, and HPV-16 infection can produce cervical dysplasia and invasive cervical cancer." [8] "At least 30 HPV types infect the genital area, of which 15 are classified as high risk, that is, having oncogenic potential"[9]
Recent studies have suggested that condoms are not highly effective in preventing HPV infection.
Cervical cancer
Epidemiologic studies combined with mathematical modelling indicate that universal vaccination of young women is likely to markedly decrease the incidence of cervical cancer.[9]
HIV
Unlike the other venereal diseases discussed here, human immunodeficiency viruses does not affect the appearance of the genitals or other entry site into the body. Instead, there is a systemic infection that lodges in a certain type of white blood cell, the lymphocyte, of the new host.
References
- ↑ Gerbase AC, Rowley JT, Mertens TE (1998), "Global epidemiology of sexually transmitted diseases", Lancet 351 (suppl III): 2–4
- ↑ :Ligon BL (2005 Oct), "Albert Ludwig Sigesmund Neisser: discoverer of the cause of gonorrhea.", Seminars in Pediatric Infectious Diseases 16 (4): 336-41
- ↑ Oriel JD (1996 Oct. UI), "The history of non-gonococcal urethritis", Genitourinary Medicine 72( (5): 374-9
- ↑ Chapter 280- GONOCOCCAL INFECTIONS in H. David Humes, Herbert L. DuPont et al (Eds) :Kelley's textbook of internal medicine.—4th ed.ISBN 0781717876
- ↑ Erdem G. Schleiss MR (2000 Jan), "Gonococcal bacteremia in a neonate", Clinical Pediatrics 39 (1): 43-4
- ↑ Bushnell, Andrew C (2 October 2007), "Lymphogranuloma Venereum", eMedicine
- ↑ Waite, Ken B (27 March 2008), "Ureaplasma infections", eMedicine
- ↑ Reichman, Richard C., Chapter 169. Human Papillomavirus Infections, Harrison's Principles of Internal Medicine, 16th Edition
- ↑ 9.0 9.1 Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, et al., DOI:10.1371/journal.pmed.0030138, at 138