Herpes: Difference between revisions
imported>Nancy Sculerati No edit summary |
mNo edit summary |
||
| (97 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
{{subpages}} | |||
'''Herpes''', also called '''herpes simplex''', is any of the diseases caused by [[herpes simplex virus]] (HSV). Symptomatic herpes simplex infections most commonly take one of two clinical forms, either a recurrent rash of swollen blisters in the area of the mouth, or a similar rash in the area of the genitals. It is possible for a single individual to have both forms of this disease. | |||
Herpes | |||
There are two subtypes ''of the virus'' that can each be responsible for either [[Herpes labialis|cold sore]]s or genital herpes; although [[human herpesvirus 1]] (herpes simplex virus-type 1 or HSV-1) is the overwhelmingly common cause of cold sores, and HSV-2 is responsible for a slight majority of genital herpes cases. Genital herpes is considered a [[STD|sexually transmitted disease]] (STD), but both types of HSV virus can be spread by both sexual ''and'' non-sexual contact. | |||
(ref for quote: | |||
"All of the herpes viruses share the characteristic of becoming latent after primary infection; the virus may subsequently reactivate periodically and produce clinical symptoms in certain individuals. The phenomenon of latent infection permits long-term persistence of the virus within the host and potential future transmissibility to others."<ref>Paula W. Annunziato: Chapter 15 – Herpes Simplex Virus Infections'' in ''Gershon: Krugman's Infectious Diseases of Children, 11th ed. Mosby, 2004</ref> ''Other'' species of Herpes virus are also human pathogens, notably [[Herpes Zoster]], the cause of both [[chicken pox]] (in acute infection) and [[shingles]] (chronic infection with reactivation). However, most commonly, the word "herpes" refers to conditions caused by Herpes simplex. | |||
== The virus == | |||
Herpes simplex virus (HSV) is a member of the ''[[Herpesviridae]]'' family of viruses, a family of DNA viruses. "Eight herpes viruses have been isolated from humans: herpes simplex virus (HSV)-1, HSV-2, human cytomegalovirus (CMV), varicella-zoster virus (VZV), Epstein-Barr virus (EBV), human herpesvirus (HHV)-6, HHV-7 and HHV-8." <ref>Yoshikawa T. Significance of human herpes viruses to transplant recipients. [Review] [45 refs] [Journal Article. Review] Current Opinion in Infectious Diseases. 16(6):601-6, 2003 Dec</ref> | |||
UI: 14624112) HSV 1 and 2 correspond to HHV 1 and 2, and both are very prevalent in the human population, with as many as 30-70% of all people tested testing positive for antibodies at some point in their lifetime. | |||
HSV's genome is a double stranded linear DNA, with about 50% sequence homology between HSV-1 and HSV-2. Many of the polypeptides produced by each type of virus are identical, and are coded by the homologous regions of DNA, but some of the expressed proteins are different and some of these distinct proteins are antigenic - that is, they give rise to an antibody response in infected hosts. Serological testing for such antibodies is the usual means to determine the type of HSV (1 or 2) infection present in patients. That means that blood tests can detect, indirectly, whether a person is infected with HSV-1 or HSV-2. | |||
== Natural history of human infection == | |||
HSV 1 and 2 are DNA viruses that have a similar route of infection, and natural history. In both types, once infection is established: it is life-long. | |||
*The route of infection is by direct contact from another person shedding the virus. | |||
*The virus enters breaks in the skin or mucus membranes. | |||
*Active replication of the virus in these cells results in the lesions of typical vesicles and shedding of the virus. | |||
*The body mounts an immunologic response and produces virus-specific killer T-cells. | |||
*The virus is destroyed, ''except'' for virus which, through retrograde axonal transport, is sequestered in the ganglion of sensory neurons. In oral "cold sores", this is usually the Trigeminal ganglion. | |||
*All symptoms of infection disappear at that point and the infected person enters a period of "latent infection". | |||
*Even during latent infections, when there are no symptoms or signs of illness, the virus is maintained in a repressed state in nerve cells. During this time, special tests done in research can demonstrate single strand viral RNA in the infected nerves. | |||
*"Reactivation of infectious virus from latent infection of trigeminal ganglia is the basis of recurrent ocular and oral HSV infection."(reference for quote: Tenser RB. Trigeminal neuralgia: mechanisms of treatment. [Review] [49 refs] [Journal Article. Review] Neurology. 51(1):17-9, 1998 Jul. UI: 9674772), and reactivation of the virus from sacral nerves is the basis for recurrent genital herpes. | |||
*The factors that cause reactivation are not completely understood. However, immunosuppression does tend to promote herpes outbreaks. | |||
Herpes Simplex viruses generally cause mucocutaneous infection, that is, cells of the ''skin'' and the ''mucous membranes'' are infected. This can manifest as cold sores on the lips, or as genital sores. The typical rash has been described as "dew drops on a rose petal", it consists of vesicles (blisters) that are initially clear and then crust over, typically with yellowish exudate. These vesicles are generally painful, and further, the area of skin and/or mucosa and the subcutaneous tissues in the region where the rash will appear commonly becomes sensitive and even swollen before eruption of the vesicles. Tissue swelling may increase as the rash blossoms, and then, generally over a course of a week to 2 weeks, resolves completely - leaving no scarring. | |||
The initial infection with the virus is called the primary infection, and can be accompanied by systemic systems such as fever and muscle aches. After resolution of the symptoms of the primary infection, the virus becomes dormant in the human host. Under certain conditions that are not well understood, the virus is reactivated, with a recurrence of mucocutaneous lesions. These recurrent attacks are unpredictable and can be frequent or infrequent. However, decreased host resistance is often correlated with recurrent attacks. The name "cold sore" for the typical Herpes simplex 1 lesion on the lip comes about because the sores will appear with the onset of an unrelated upper respiratory virus, and these lesions also recur in times of stress and other illnesses. However, recurrences can occur even when the infected person feels well and is under no apparent stress. | |||
In general, lesions from HSV 1 are more commonly seen on the face, but also accounts for a large minority of genital infections. HSV 2 lesions are much more commonly seen on the genitalia than the face. Although genital lesions are a form of STD, other lesions can be contracted without sexual contact. Regardless of how they were contracted, however, an infected person can spread virus to another person with mucosa to mucosa or skin to mucosa contact. | |||
Transmission can occur when sores are visible, as well as when there are no visible lesions. In addition to the common mucocutaneous infection, HSV 1 and 2 can also cause keratitis (inflammation in the eye), encephalitis (brain infection), and severe neonatal disease if acquired during pregnancy. | |||
==Diagnosis== | |||
The diagnosis of a herpes simplex infection is ordinarily a clinical one, that is- it is made by a trained health care provider based on the patient's history and physical findings, rather than on laboratory tests. However, a clinical diagnosis does not distinguish between HSV-1 and HSV-2 infection, except by probability. Confirming a diagnosis and clarifying the actual virus type involve requires laboratory testing. The most definitive proof of infection, the "gold standard" of diagnostic tests, is the growth of the virus in artificial culture from a specimen taken from the patient's lesions. Although primary ulcers have a high rate of viral shed, recurrent lesions shed virus at a much lower rate, and so culture of recurrent lesions has a high false negative rate. Accordingly, in patients with typical presentations of recurrent outbreaks, failure to culture the virus in no way overturns the diagnosis. | |||
Viral culture is an expensive laboratory test that must be carried out for 10 days in order to assume negative results. | |||
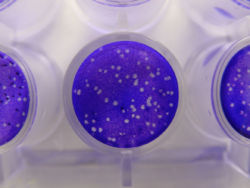
{{Image|Plaque assay macro.jpg|right|250px|These cell culture dishes are pictured from a laboratory performing culture of herpes simplex virus. Viral plaque formation: Vero cells, were grown to completely cover the bottom of the plastic plate (1.5 cm diameter), and then were infected with herpes simplex virus (approximately 75 plaque forming unit) and then cultured overnight. At the time of the photograph, a vital dye (crystal violet) had been placed in the culture dishes. Living cels take up the dye and are purple. Cells that have been killed by viruses are called viral plaques, and no dye can be transported in to stain them: they remain transparent. Each plaque was formed from one virion.}} | |||
"PCR techniques are more sensitive than viral cuture and results can be available in less than 4 hours". <ref>Sullivan M. Sams R 2nd. Jamieson B. Holt J. Clinical inquiries. What is the best test to detect herpes in skin lesions?. Journal of Family Practice. 55(4):346, 348, 2006 Apr.)</ref> | |||
Diagnostic tests on the immune response to the virus can determine not only the subtype of herpes simplex infection but whether the outbreak is primary or recurrent. | |||
HSV-1 and HSV-2 each have respective variations in virally produced glycoprotein G, and immunoglobulin G (IgG) produced by an infected person differs accordingly. If an individual is making IgG to either type of virus, 1 or 2, infection is confirmed. If the individual has clear signs of a genital herpes infection, but the tests for IGG are negative, the most likely explanation is that this is a primary outbreak, and the patient has not yet begun production of that type of antibody. Confirmation of that presumed diagnosis of a primary herpes infection can be made on follow-up testing, with demonstration of anti-HSV IgG levels. | |||
==Oral herpes infection== | |||
{{Image|Herpes labialis - opryszczka wargowa.jpg|left|350px| Cold sores are most commonly caused by [[Human herpesvirus 1]] and are ubiquitous in distribution in human populations. Here, the vesicles have crusted over and begun to heal.}} | |||
Oral herpes simplex infections include [[Herpes labialis]] and [[Herpetic stomatitis]]. | |||
==Genital herpes infection== | |||
In population studies in the United States, both serotypes of the herpes virus are prevalent in symptomatic genital herpes infections. HSV-2 accounting for more than half, and HSV-1 for almost half, of all infections. More than 50 million people are infected in that country, making this the most common STD in the USA. | |||
Although both types of herpes simplex virus can account for genital herpes, and cause a very similar appearing rash, "HSV-1 has a much lower recurrence rate. For example, 40% of patients with an initial episode of HSV-1 will remain asymptomatic during the first year of infection, while 40% of patients with an initial outbreak of HSV-2 will have six or more recurrences per year." <ref>Kirkland LG. New developments in the management of STDs. [Review] [10 refs] [Journal Article. Review] Nurse Practitioner. 31(12):12-21; quiz 22-3, 2006 Dec. UI: 17149130</ref> | |||
The Center for Disease Control (CDC) in the United States recommends that genital lesions be cultured in order to determine the type of HSV infection, since the severity and clinical course of the disease can be better predicted with this information. | |||
There is a relationship between genital herpes and the risk of catching (and spreading) additional venereal diseases, since the ulcers caused by herpes are more vulnerable to invasion by pathogens than intact skin or mucosa. In the case of AIDS, "the presence of genital ulcers increases the transmission of HIV, and the presence of HIV adversely affects the natural history of HSV infection." <ref>Severson JL. Tyring SK. Relation between herpes simplex viruses and human immunodeficiency virus infections. Archives of Dermatology. 135(11):1393-7, 1999 Nov. | |||
UI: 10566840</ref> Since AIDS causes weakened immunity, herpes outbreaks (both oral and genital) can become more frequent. | |||
==Ophthalmologic herpes simplex infection (eye)== | |||
"Herpetic eye disease is among the most common causes for infectious uveitis. It may affect healthy as well as immune-compromised hosts, although its clinical presentation varies accordingly." | |||
==Herpes encephalitis== | |||
==Herpes simplex infection in neonates== | |||
Although herpes infection is aggravating in healthy adults, it is a lethal disease in very young babies. | |||
"Neonatal HSV disease is acquired at 1 of 3 distinct times: intrauterine (in utero); peripartum (perinatal); and postpartum (postnatal)" <ref>Kimberlin DW. Diagnosis of herpes simplex virus in the era of polymerase chain reaction. Pediatric Infectious Disease Journal. 25(9):841-2, 2006 Sep.</ref> Among pregnant women in the United States, "greater than 60% are positive for HSV-1...Overall, 60–80% of neonatal herpes is associated with the primary or first-episode genital herpes acquired in close proximity to delivery."<ref>Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252</ref> | |||
"maternal acquisition of new infection in late pregnancy, ... accounts for 60–80% of neonatal herpes"<ref>Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252</ref> | |||
However, newborns have a limited immune system for the first 3 weeks of life, and even a kiss by a well-meaning friend or relative who bears a virus-shedding cold sore on the lips can cause infection in the newborn (albeit rarely). | |||
==Transplant patients== | |||
All the immunosuppressive drugs used to allow transplant patients to keep their transplanted organs healthy have an unfortunate side effect of reactivating latent herpes simplex infections. | |||
== Prevention and treatment == | |||
There is currently no vaccine available for either virus. Because HSV 2 is spread more commonly by sexual contact, it is easier to prevent than HSV 1. Avoiding contact with people who have obvious sores helps reduce infection, and prophylaxis with commonly available antiviral drugs can help prevent transmission during the latent phase of the illness. Prophylaxis can also be given to reduce frequency and severity of attacks. Consistent and correct use of condoms reduces genital transmission. | |||
==History== | |||
Herpes has been recognized for centuries, "cold sores" (''herpes febrilis'') were described by the Roman physician [[Herodotus]] in the year 100 CE. Genital herpes was first described by [[John Astruc]], physician to the king of France, in 1736, and the first English translation appeared in his treatise on venereal disease in 1754." | |||
HSV was first grown ''in vitro'' in 1925. | |||
== References == | == References == | ||
<references/> | |||
Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company | : Goldman: Cecil ''Textbook of Medicine'', 22nd ed., Copyright © 2004 W. B. Saunders Company | ||
[[Category: | : Cohen & Powderly: ''Infectious Diseases'', 2nd ed., Copyright © 2004 Mosby, An Imprint of Elsevier[[Category:Suggestion Bot Tag]] | ||
Latest revision as of 11:01, 27 August 2024
Herpes, also called herpes simplex, is any of the diseases caused by herpes simplex virus (HSV). Symptomatic herpes simplex infections most commonly take one of two clinical forms, either a recurrent rash of swollen blisters in the area of the mouth, or a similar rash in the area of the genitals. It is possible for a single individual to have both forms of this disease.
There are two subtypes of the virus that can each be responsible for either cold sores or genital herpes; although human herpesvirus 1 (herpes simplex virus-type 1 or HSV-1) is the overwhelmingly common cause of cold sores, and HSV-2 is responsible for a slight majority of genital herpes cases. Genital herpes is considered a sexually transmitted disease (STD), but both types of HSV virus can be spread by both sexual and non-sexual contact.
(ref for quote:
"All of the herpes viruses share the characteristic of becoming latent after primary infection; the virus may subsequently reactivate periodically and produce clinical symptoms in certain individuals. The phenomenon of latent infection permits long-term persistence of the virus within the host and potential future transmissibility to others."[1] Other species of Herpes virus are also human pathogens, notably Herpes Zoster, the cause of both chicken pox (in acute infection) and shingles (chronic infection with reactivation). However, most commonly, the word "herpes" refers to conditions caused by Herpes simplex.
The virus
Herpes simplex virus (HSV) is a member of the Herpesviridae family of viruses, a family of DNA viruses. "Eight herpes viruses have been isolated from humans: herpes simplex virus (HSV)-1, HSV-2, human cytomegalovirus (CMV), varicella-zoster virus (VZV), Epstein-Barr virus (EBV), human herpesvirus (HHV)-6, HHV-7 and HHV-8." [2] UI: 14624112) HSV 1 and 2 correspond to HHV 1 and 2, and both are very prevalent in the human population, with as many as 30-70% of all people tested testing positive for antibodies at some point in their lifetime.
HSV's genome is a double stranded linear DNA, with about 50% sequence homology between HSV-1 and HSV-2. Many of the polypeptides produced by each type of virus are identical, and are coded by the homologous regions of DNA, but some of the expressed proteins are different and some of these distinct proteins are antigenic - that is, they give rise to an antibody response in infected hosts. Serological testing for such antibodies is the usual means to determine the type of HSV (1 or 2) infection present in patients. That means that blood tests can detect, indirectly, whether a person is infected with HSV-1 or HSV-2.
Natural history of human infection
HSV 1 and 2 are DNA viruses that have a similar route of infection, and natural history. In both types, once infection is established: it is life-long.
- The route of infection is by direct contact from another person shedding the virus.
- The virus enters breaks in the skin or mucus membranes.
- Active replication of the virus in these cells results in the lesions of typical vesicles and shedding of the virus.
- The body mounts an immunologic response and produces virus-specific killer T-cells.
- The virus is destroyed, except for virus which, through retrograde axonal transport, is sequestered in the ganglion of sensory neurons. In oral "cold sores", this is usually the Trigeminal ganglion.
- All symptoms of infection disappear at that point and the infected person enters a period of "latent infection".
- Even during latent infections, when there are no symptoms or signs of illness, the virus is maintained in a repressed state in nerve cells. During this time, special tests done in research can demonstrate single strand viral RNA in the infected nerves.
- "Reactivation of infectious virus from latent infection of trigeminal ganglia is the basis of recurrent ocular and oral HSV infection."(reference for quote: Tenser RB. Trigeminal neuralgia: mechanisms of treatment. [Review] [49 refs] [Journal Article. Review] Neurology. 51(1):17-9, 1998 Jul. UI: 9674772), and reactivation of the virus from sacral nerves is the basis for recurrent genital herpes.
- The factors that cause reactivation are not completely understood. However, immunosuppression does tend to promote herpes outbreaks.
Herpes Simplex viruses generally cause mucocutaneous infection, that is, cells of the skin and the mucous membranes are infected. This can manifest as cold sores on the lips, or as genital sores. The typical rash has been described as "dew drops on a rose petal", it consists of vesicles (blisters) that are initially clear and then crust over, typically with yellowish exudate. These vesicles are generally painful, and further, the area of skin and/or mucosa and the subcutaneous tissues in the region where the rash will appear commonly becomes sensitive and even swollen before eruption of the vesicles. Tissue swelling may increase as the rash blossoms, and then, generally over a course of a week to 2 weeks, resolves completely - leaving no scarring.
The initial infection with the virus is called the primary infection, and can be accompanied by systemic systems such as fever and muscle aches. After resolution of the symptoms of the primary infection, the virus becomes dormant in the human host. Under certain conditions that are not well understood, the virus is reactivated, with a recurrence of mucocutaneous lesions. These recurrent attacks are unpredictable and can be frequent or infrequent. However, decreased host resistance is often correlated with recurrent attacks. The name "cold sore" for the typical Herpes simplex 1 lesion on the lip comes about because the sores will appear with the onset of an unrelated upper respiratory virus, and these lesions also recur in times of stress and other illnesses. However, recurrences can occur even when the infected person feels well and is under no apparent stress.
In general, lesions from HSV 1 are more commonly seen on the face, but also accounts for a large minority of genital infections. HSV 2 lesions are much more commonly seen on the genitalia than the face. Although genital lesions are a form of STD, other lesions can be contracted without sexual contact. Regardless of how they were contracted, however, an infected person can spread virus to another person with mucosa to mucosa or skin to mucosa contact.
Transmission can occur when sores are visible, as well as when there are no visible lesions. In addition to the common mucocutaneous infection, HSV 1 and 2 can also cause keratitis (inflammation in the eye), encephalitis (brain infection), and severe neonatal disease if acquired during pregnancy.
Diagnosis
The diagnosis of a herpes simplex infection is ordinarily a clinical one, that is- it is made by a trained health care provider based on the patient's history and physical findings, rather than on laboratory tests. However, a clinical diagnosis does not distinguish between HSV-1 and HSV-2 infection, except by probability. Confirming a diagnosis and clarifying the actual virus type involve requires laboratory testing. The most definitive proof of infection, the "gold standard" of diagnostic tests, is the growth of the virus in artificial culture from a specimen taken from the patient's lesions. Although primary ulcers have a high rate of viral shed, recurrent lesions shed virus at a much lower rate, and so culture of recurrent lesions has a high false negative rate. Accordingly, in patients with typical presentations of recurrent outbreaks, failure to culture the virus in no way overturns the diagnosis.
Viral culture is an expensive laboratory test that must be carried out for 10 days in order to assume negative results.
"PCR techniques are more sensitive than viral cuture and results can be available in less than 4 hours". [3]
Diagnostic tests on the immune response to the virus can determine not only the subtype of herpes simplex infection but whether the outbreak is primary or recurrent. HSV-1 and HSV-2 each have respective variations in virally produced glycoprotein G, and immunoglobulin G (IgG) produced by an infected person differs accordingly. If an individual is making IgG to either type of virus, 1 or 2, infection is confirmed. If the individual has clear signs of a genital herpes infection, but the tests for IGG are negative, the most likely explanation is that this is a primary outbreak, and the patient has not yet begun production of that type of antibody. Confirmation of that presumed diagnosis of a primary herpes infection can be made on follow-up testing, with demonstration of anti-HSV IgG levels.
Oral herpes infection

Oral herpes simplex infections include Herpes labialis and Herpetic stomatitis.
Genital herpes infection
In population studies in the United States, both serotypes of the herpes virus are prevalent in symptomatic genital herpes infections. HSV-2 accounting for more than half, and HSV-1 for almost half, of all infections. More than 50 million people are infected in that country, making this the most common STD in the USA.
Although both types of herpes simplex virus can account for genital herpes, and cause a very similar appearing rash, "HSV-1 has a much lower recurrence rate. For example, 40% of patients with an initial episode of HSV-1 will remain asymptomatic during the first year of infection, while 40% of patients with an initial outbreak of HSV-2 will have six or more recurrences per year." [4]
The Center for Disease Control (CDC) in the United States recommends that genital lesions be cultured in order to determine the type of HSV infection, since the severity and clinical course of the disease can be better predicted with this information.
There is a relationship between genital herpes and the risk of catching (and spreading) additional venereal diseases, since the ulcers caused by herpes are more vulnerable to invasion by pathogens than intact skin or mucosa. In the case of AIDS, "the presence of genital ulcers increases the transmission of HIV, and the presence of HIV adversely affects the natural history of HSV infection." [5] Since AIDS causes weakened immunity, herpes outbreaks (both oral and genital) can become more frequent.
Ophthalmologic herpes simplex infection (eye)
"Herpetic eye disease is among the most common causes for infectious uveitis. It may affect healthy as well as immune-compromised hosts, although its clinical presentation varies accordingly."
Herpes encephalitis
Herpes simplex infection in neonates
Although herpes infection is aggravating in healthy adults, it is a lethal disease in very young babies.
"Neonatal HSV disease is acquired at 1 of 3 distinct times: intrauterine (in utero); peripartum (perinatal); and postpartum (postnatal)" [6] Among pregnant women in the United States, "greater than 60% are positive for HSV-1...Overall, 60–80% of neonatal herpes is associated with the primary or first-episode genital herpes acquired in close proximity to delivery."[7]
"maternal acquisition of new infection in late pregnancy, ... accounts for 60–80% of neonatal herpes"[8]
However, newborns have a limited immune system for the first 3 weeks of life, and even a kiss by a well-meaning friend or relative who bears a virus-shedding cold sore on the lips can cause infection in the newborn (albeit rarely).
Transplant patients
All the immunosuppressive drugs used to allow transplant patients to keep their transplanted organs healthy have an unfortunate side effect of reactivating latent herpes simplex infections.
Prevention and treatment
There is currently no vaccine available for either virus. Because HSV 2 is spread more commonly by sexual contact, it is easier to prevent than HSV 1. Avoiding contact with people who have obvious sores helps reduce infection, and prophylaxis with commonly available antiviral drugs can help prevent transmission during the latent phase of the illness. Prophylaxis can also be given to reduce frequency and severity of attacks. Consistent and correct use of condoms reduces genital transmission.
History
Herpes has been recognized for centuries, "cold sores" (herpes febrilis) were described by the Roman physician Herodotus in the year 100 CE. Genital herpes was first described by John Astruc, physician to the king of France, in 1736, and the first English translation appeared in his treatise on venereal disease in 1754."
HSV was first grown in vitro in 1925.
References
- ↑ Paula W. Annunziato: Chapter 15 – Herpes Simplex Virus Infections in Gershon: Krugman's Infectious Diseases of Children, 11th ed. Mosby, 2004
- ↑ Yoshikawa T. Significance of human herpes viruses to transplant recipients. [Review] [45 refs] [Journal Article. Review] Current Opinion in Infectious Diseases. 16(6):601-6, 2003 Dec
- ↑ Sullivan M. Sams R 2nd. Jamieson B. Holt J. Clinical inquiries. What is the best test to detect herpes in skin lesions?. Journal of Family Practice. 55(4):346, 348, 2006 Apr.)
- ↑ Kirkland LG. New developments in the management of STDs. [Review] [10 refs] [Journal Article. Review] Nurse Practitioner. 31(12):12-21; quiz 22-3, 2006 Dec. UI: 17149130
- ↑ Severson JL. Tyring SK. Relation between herpes simplex viruses and human immunodeficiency virus infections. Archives of Dermatology. 135(11):1393-7, 1999 Nov. UI: 10566840
- ↑ Kimberlin DW. Diagnosis of herpes simplex virus in the era of polymerase chain reaction. Pediatric Infectious Disease Journal. 25(9):841-2, 2006 Sep.
- ↑ Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252
- ↑ Tita AT. Grobman WA. Rouse DJ. Antenatal herpes serologic screening: an appraisal of the evidence. [Review] [49 refs] [Journal Article. Review] Obstetrics & Gynecology. 108(5):1247-53, 2006 Nov. UI: 17077252
- Goldman: Cecil Textbook of Medicine, 22nd ed., Copyright © 2004 W. B. Saunders Company
- Cohen & Powderly: Infectious Diseases, 2nd ed., Copyright © 2004 Mosby, An Imprint of Elsevier