Lissencephaly: Difference between revisions
imported>Daniel Mietchen (restructured) |
imported>Daniel Mietchen |
||
| (12 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{subpages}} | {{subpages}} | ||
{{Image|Brain-disease-gyrification.png|right|400px|Gyrification from a clinical perspective: Normal adulthuman [[cerebral cortex|cortical surface]] (left), [[polymicrogyria]] (center) and lissencephaly (right).}} | |||
{{TOC|right}} | |||
In general, '''lissencephaly''' describes the shape of a brain as being smooth, as opposed to [[gyrification|gyrified]]. This means that [[sulcus|cortical fissures]] | In general, '''lissencephaly''' describes the shape of a brain as being smooth, as opposed to [[gyrification|gyrified]]. This means that [[sulcus|cortical fissures]] are less pronounced than, for instance, in the adult human brain (a condition known as [[pachygyria]]), or even totally absent ([[agyria]]). The term is used both in the medical sense of describing a [[neurodevelopmental disorder]] due to disturbed [[neuronal migration]] during the [[brain development|development]] of the [[cerebral cortex]], and in the more general [[comparative biology|comparative biological]] sense of describing brains with low degrees of [[gyrification|cortical convolution]]. | ||
In | ==Lissencephaly as a developmental disorder== | ||
In human infants, lissencephaly develops during the 12th to 24th weeks of [[gestation]], resulting in disturbed [[cortical connectivity]] and accompanying lack of development of brain folds ([[gyrus|gyri]]) and grooves ([[sulcus|sulci]]).<ref>Dobyns, WB. ''Developmental aspects of lissencephaly and the lissencephaly syndromes.'' Birth Defects Orig Artic Ser 1987; 23:225.</ref> It is a form of [[cephalic disorder]]. Terms such as '[[agyria]]' (no gyri) or '[[pachygyria]]' (broad gyri) are used to describe the appearance of the surface of the brain. Histologically, lissencephalic brains are characterized by a significant reduction (or even complete lack) of layers II and IV of the [[cerebral cortex]]. Children with lissencephaly are severely neurologically impaired<ref>Bauman, ML. Neuroembryology--clinical aspects. Semin Perinatol 1987; 11:74.</ref> and often die within several months of birth.<ref name=Jones2006>Jones, KL. ''Smith's Recognizable Patterns of Human Malformation, 6th ed.'' Elsevier Saunders, Philadelphia 2006.</ref> | |||
In other [[mammal]]s, particularly those with [[brain size|small brains]], lissencephaly | ===Symptoms=== | ||
Affected children display severe psychomotor retardation, [[failure to thrive]], [[seizure]]s, and muscle [[spasticity]] or [[hypotonia]].<ref name=Jones2006/> Other symptoms of the disorder may include unusual facial appearance, difficulty swallowing, and anomalies of the hands, [[finger]]s, or [[toe]]s. | |||
===Diagnosis=== | |||
The diagnosis of lissencephaly is usually made at birth or soon after by [[ultrasound]], [[computed tomography]] (CT), or [[magnetic resonance imaging]] (MRI). Before birth, complex ultrasounds performed routinely during pregnancy may indicate the presence of cerebral abnormality, but this method of diagnosis is not reliable, and an absence of abnormal cerebral pathology should only inspire cautious optimism at best. In any case, diagnosis by ultrasound probably cannot be reliably made until 26 to 28 weeks, when the normal gyri and sulci become well defined. Up to this time, the fetal brain normally has a smooth appearance.<ref>Dorovini-Zis K; Dolman CL. Gestational development of brain. Archives of Pathologic Laboratory Medicine 1977 Apr;101(4):192-5.</ref> If lissencephaly is suspected, [[chorionic villus sampling]] can test for some lissencephaly variants, but only those with a known genetic mutation. | |||
===Causes=== | |||
Causes of lissencephaly can include [[virus|viral]] infections of the uterus or the fetus during the first trimester, or insufficient blood supply to the fetal brain early in pregnancy. There are also a number of genetic causes of lissencephaly, including mutation of the [[reelin]] gene (on [[chromosome 7]]),<ref>Hong SE, Shugart YY, Huang DT, Shahwan SA, Grant PE, Hourihane JO, Martin ND, Walsh CA. (2000) ''Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations.'' Nat Genet. 26(1):93-6. PMID 10973257<br></ref> as well as other genes on the [[X chromosome]] and on [[chromosome 17]]. [[Genetic counseling]] is usually offered if there is a risk of lissencephaly, coupled with [[genetic testing]]. | |||
===Classification=== | |||
The spectrum of lissencephaly is only now becoming more defined as neuroimaging and [[genetics]] has provided more insights into migration disorders. There are around 20 different types of lissencephaly which make up the spectrum. Other causes which have not yet been identified are likely as well. | |||
Different systems for classifying lissencephaly exist. One major distinction is "classic" (type I) vs. "cobblestone" (type II),<ref name="pmid16215456">{{cite journal |author=Forman MS, Squier W, Dobyns WB, Golden JA |title=Genotypically defined lissencephalies show distinct pathologies |journal=J. Neuropathol. Exp. Neurol. |volume=64 |issue=10 |pages=847–57 |year=2005 |month=October |pmid=16215456 |doi= |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0022-3069&volume=64&issue=10&spage=847}}</ref> but some systems add additional forms that fit into neither of these categories. | |||
<!-- | |||
Some types of lissencephaly are described below ([[OMIM]] numbers are included where available): | |||
{| class="wikitable" | |||
| '''Category''' || '''Types''' | |||
|- | |||
| Classic (or Type 1) lissencephaly - {{OMIM2|607432}} || | |||
* LIS1: lissencephaly due to [[PAFAH1B1]] gene mutation, which subdivides into: | |||
** type 1 isolated lissencephaly ({{OMIM2|601545}}) | |||
** [[Miller-Dieker syndrome]] ({{OMIM2|247200}}) | |||
* LISX1: lissencephaly due to [[doublecortin]] (DCX) gene mutation ({{OMIM2|300121}}) | |||
* lissencephaly, type 1, isolated, without other known genetic defects | |||
* | |||
|- | |||
| Cobblestone (or Type 2) lissencephaly || | |||
* [[Walker-Warburg syndrome]] ({{OMIM2|236670}}), also called HARD(E) syndrome | |||
* [[Fukuyama syndrome]] ({{OMIM2|253800}}) | |||
* [[Muscle-eye-brain disease]] (MEB) ({{OMIM2|253280}}) | |||
|- | |||
| Other types || | |||
* LIS2: [[Norman-Roberts syndrome]] (mutation of [[reelin]] gene, {{OMIM2|257320}}) | |||
* LIS3: [[TUBA1A]], {{OMIM2|611603}} | |||
* LISX2: [[Aristaless related homeobox|ARX]], {{OMIM2|300215}} | |||
* Microlissencephaly (lissencephaly and [[microcephaly]])<ref>[http://www.orpha.net/static/GB/microlissencephaly.html Microlissencephaly]</ref> | |||
|} | |||
--> | |||
===Treatment=== | |||
Treatment for those with lissencephaly is symptomatic and depends on the severity and locations of the brain malformations. Supportive care may be needed to help with comfort and nursing needs. Seizures may be controlled with medication and hydrocephalus may require shunting. If feeding becomes difficult, a [[gastrostomy]] tube may be considered. | |||
===Prognosis=== | |||
The prognosis for children with lissencephaly varies depending on the degree of brain malformation. Many individuals show no significant development beyond a 3- to 5-month-old level. Some may have near-normal development and [[intelligence (trait)|intelligence]]. but with modern medications and care, some children live into their teens. Respiratory problems are the most common causes of death. | |||
==Lissencephaly from a comparative perspective== | |||
In other [[mammal]]s, particularly those with [[brain size|small brains]], lissencephaly is generally the normal state of an adult brain, as is the case with [[beaver]]s, [[manatee]]s and [[platypus]]es, for instance. This is opposed to [[gyrencephaly|gyrencephalic]] brains, characterized by a high degree of gyrification, which is commonly found in larger brains. | |||
==References== | |||
{{reflist|2}} | |||
Latest revision as of 21:31, 9 July 2011
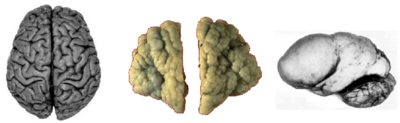
Gyrification from a clinical perspective: Normal adulthuman cortical surface (left), polymicrogyria (center) and lissencephaly (right).
In general, lissencephaly describes the shape of a brain as being smooth, as opposed to gyrified. This means that cortical fissures are less pronounced than, for instance, in the adult human brain (a condition known as pachygyria), or even totally absent (agyria). The term is used both in the medical sense of describing a neurodevelopmental disorder due to disturbed neuronal migration during the development of the cerebral cortex, and in the more general comparative biological sense of describing brains with low degrees of cortical convolution.
Lissencephaly as a developmental disorder
In human infants, lissencephaly develops during the 12th to 24th weeks of gestation, resulting in disturbed cortical connectivity and accompanying lack of development of brain folds (gyri) and grooves (sulci).[1] It is a form of cephalic disorder. Terms such as 'agyria' (no gyri) or 'pachygyria' (broad gyri) are used to describe the appearance of the surface of the brain. Histologically, lissencephalic brains are characterized by a significant reduction (or even complete lack) of layers II and IV of the cerebral cortex. Children with lissencephaly are severely neurologically impaired[2] and often die within several months of birth.[3]
Symptoms
Affected children display severe psychomotor retardation, failure to thrive, seizures, and muscle spasticity or hypotonia.[3] Other symptoms of the disorder may include unusual facial appearance, difficulty swallowing, and anomalies of the hands, fingers, or toes.
Diagnosis
The diagnosis of lissencephaly is usually made at birth or soon after by ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI). Before birth, complex ultrasounds performed routinely during pregnancy may indicate the presence of cerebral abnormality, but this method of diagnosis is not reliable, and an absence of abnormal cerebral pathology should only inspire cautious optimism at best. In any case, diagnosis by ultrasound probably cannot be reliably made until 26 to 28 weeks, when the normal gyri and sulci become well defined. Up to this time, the fetal brain normally has a smooth appearance.[4] If lissencephaly is suspected, chorionic villus sampling can test for some lissencephaly variants, but only those with a known genetic mutation.
Causes
Causes of lissencephaly can include viral infections of the uterus or the fetus during the first trimester, or insufficient blood supply to the fetal brain early in pregnancy. There are also a number of genetic causes of lissencephaly, including mutation of the reelin gene (on chromosome 7),[5] as well as other genes on the X chromosome and on chromosome 17. Genetic counseling is usually offered if there is a risk of lissencephaly, coupled with genetic testing.
Classification
The spectrum of lissencephaly is only now becoming more defined as neuroimaging and genetics has provided more insights into migration disorders. There are around 20 different types of lissencephaly which make up the spectrum. Other causes which have not yet been identified are likely as well.
Different systems for classifying lissencephaly exist. One major distinction is "classic" (type I) vs. "cobblestone" (type II),[6] but some systems add additional forms that fit into neither of these categories.
Treatment
Treatment for those with lissencephaly is symptomatic and depends on the severity and locations of the brain malformations. Supportive care may be needed to help with comfort and nursing needs. Seizures may be controlled with medication and hydrocephalus may require shunting. If feeding becomes difficult, a gastrostomy tube may be considered.
Prognosis
The prognosis for children with lissencephaly varies depending on the degree of brain malformation. Many individuals show no significant development beyond a 3- to 5-month-old level. Some may have near-normal development and intelligence. but with modern medications and care, some children live into their teens. Respiratory problems are the most common causes of death.
Lissencephaly from a comparative perspective
In other mammals, particularly those with small brains, lissencephaly is generally the normal state of an adult brain, as is the case with beavers, manatees and platypuses, for instance. This is opposed to gyrencephalic brains, characterized by a high degree of gyrification, which is commonly found in larger brains.
References
- ↑ Dobyns, WB. Developmental aspects of lissencephaly and the lissencephaly syndromes. Birth Defects Orig Artic Ser 1987; 23:225.
- ↑ Bauman, ML. Neuroembryology--clinical aspects. Semin Perinatol 1987; 11:74.
- ↑ 3.0 3.1 Jones, KL. Smith's Recognizable Patterns of Human Malformation, 6th ed. Elsevier Saunders, Philadelphia 2006.
- ↑ Dorovini-Zis K; Dolman CL. Gestational development of brain. Archives of Pathologic Laboratory Medicine 1977 Apr;101(4):192-5.
- ↑ Hong SE, Shugart YY, Huang DT, Shahwan SA, Grant PE, Hourihane JO, Martin ND, Walsh CA. (2000) Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations. Nat Genet. 26(1):93-6. PMID 10973257
- ↑ Forman MS, Squier W, Dobyns WB, Golden JA (October 2005). "Genotypically defined lissencephalies show distinct pathologies". J. Neuropathol. Exp. Neurol. 64 (10): 847–57. PMID 16215456. [e]