Hypertension: Difference between revisions
imported>Robert Badgett |
imported>Robert Badgett |
||
| Line 57: | Line 57: | ||
The race and age demographic may partly predict frequency of [[adverse drug respons]]es to different anti-hypertensive mediations.<ref name="pmid16679330">{{cite journal |author=McDowell SE, Coleman JJ, Ferner RE |title=Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine |journal=BMJ |volume=332 |issue=7551 |pages=1177–81 |year=2006 |pmid=16679330 |doi=10.1136/bmj.38803.528113.55}}</ref> | The race and age demographic may partly predict frequency of [[adverse drug respons]]es to different anti-hypertensive mediations.<ref name="pmid16679330">{{cite journal |author=McDowell SE, Coleman JJ, Ferner RE |title=Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine |journal=BMJ |volume=332 |issue=7551 |pages=1177–81 |year=2006 |pmid=16679330 |doi=10.1136/bmj.38803.528113.55}}</ref> | ||
==Persistent hypertension== | |||
===Systolic hypertension=== | ===Systolic hypertension=== | ||
Revision as of 22:19, 22 October 2007
Hypertension is a multisystem disease whose hallmark is the elevation of blood pressure.
Classification
| Blood pressure classification | Initial blood pressure mm Hg | Followup recommended | ||
|---|---|---|---|---|
| SBP | DBP | |||
| Normal | <120 | and | <80 | Recheck in 2 years |
| Prehypertension | 120-139 | or | 80-99 | Recheck in 1 year |
| Stage 1 Hypertension | 140-159 | or | 90-99 | Confirm within 2 months |
| Stage 2 Hypertension | >160 | or | >100 | "Evaluate or refer to source of care within 1 month. For those with higher pressures (e.g., >180/110 mmHg), evaluate and treat immediately or within 1 week depending on clinical situation and complications." |
Diagnosis
Treatment
Current clinical practice guidelines are based on The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).[1]
Treatment goals
Per the JNC7 Guidelines:[1]
- "Treating "most patients" SBP and DBP to targets that are <140/90 mmHg is associated with a decrease in cardiovascular complications.
- In patients with hypertension and diabetes or renal disease, the BP goal is <130/80 mmHg.
Initial medication
In the absence of any comordid medical conditions that would affect the selection of a drug, the JNC7 recommends:
- "Thiazide-type diuretics for most"[1]
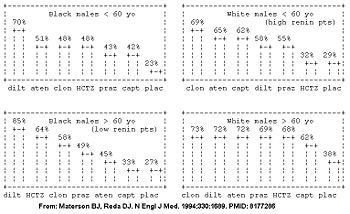
However, the initial drug may be better selected based on the patient's age, race, and gender.[2][3] The patient's demographic roughly corresponds with their renin profile, but is more predictive than the renin profile.[3] The molecular basis is being determined.[4]
In the high renin demographic (young whites), diuretics had similar efficacy to placebo; whereas in the low renin demographic (older blacks), the ace-inhibitors had similar efficacy to placebo in the Masterson Veterans Affairs Cooperative Study Group on Antihypertensive Agents (see figure).[2]
| Category name | demographics | Comments | Best anti-hypertensive categories |
|---|---|---|---|
| High renin demographic | less than 50 years old, anglo | salt-sensitive; diuretic responsive | diuretics, calcium channel blockers |
| Low renin demographic | more than 50 years old, non-anglo* | ace-inhibitors, beta-blockers | |
| * Obesity and female[5] are also associated with low renin. | |||
Several randomized controlled trials have compared initial medications for hypertension.[6][7][8][2]
- In the Second Australian National Blood Pressure study (ANBP2),[7] ace-inhibitors were better in a population that was 95% white with a body-mass index of 27. This demographic has features of both high (age) and low (race) renin status.
- In the ALLHAT study,[6] diuretics were better in a population that was 47% white with a body-mass index of 30.
For patients with Stage 2 Hypertension (SBP >160 or DBP>100 mmHg), start with two drugs.[1]
The race and age demographic may partly predict frequency of adverse drug responses to different anti-hypertensive mediations.[9]
Persistent hypertension
Systolic hypertension
Prognosis
References
- ↑ 1.0 1.1 1.2 1.3 Chobanian AV, Bakris GL, Black HR, et al (2003). "The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report". JAMA 289 (19): 2560-72. DOI:10.1001/jama.289.19.2560. PMID 12748199. Research Blogging. http://www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf
- ↑ 2.0 2.1 2.2 2.3 Materson BJ, Reda DJ (1994). "Correction: single-drug therapy for hypertension in men". N. Engl. J. Med. 330 (23): 1689. PMID 8177286. [e]
Cite error: Invalid
<ref>tag; name "pmid8177286" defined multiple times with different content - ↑ 3.0 3.1 Preston RA, Materson BJ, Reda DJ, et al (1998). "Age-race subgroup compared with renin profile as predictors of blood pressure response to antihypertensive therapy. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents". JAMA 280 (13): 1168–72. PMID 9777817. [e]
- ↑ Materson BJ (2007). "Variability in response to antihypertensive drugs". Am. J. Med. 120 (4 Suppl 1): S10–20. DOI:10.1016/j.amjmed.2007.02.003. PMID 17403377. Research Blogging.
- ↑ Cowley AW, Skelton MM, Velasquez MT (1985). "Sex differences in the endocrine predictors of essential hypertension. Vasopressin versus renin". Hypertension 7 (3 Pt 2): I151–60. PMID 3888837. [e]
- ↑ 6.0 6.1 ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (2002). "Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)". JAMA 288 (23): 2981-97. PMID 12479763. [e]
- ↑ 7.0 7.1 Wing LM, Reid CM, Ryan P, et al (2003). "A comparison of outcomes with angiotensin-converting--enzyme inhibitors and diuretics for hypertension in the elderly". N. Engl. J. Med. 348 (7): 583-92. DOI:10.1056/NEJMoa021716. PMID 12584366. Research Blogging.
- ↑ Materson BJ, Reda DJ, Cushman WC, et al (1993). "Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents". N. Engl. J. Med. 328 (13): 914-21. PMID 8446138. [e]
- ↑ McDowell SE, Coleman JJ, Ferner RE (2006). "Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine". BMJ 332 (7551): 1177–81. DOI:10.1136/bmj.38803.528113.55. PMID 16679330. Research Blogging.