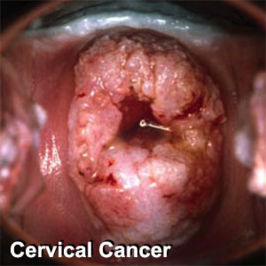
Cervical cancer
Screening
Clinical practice guidelines
Clinical practice guidelines by the U.S. Preventive Services Task Force guide screening:[1]
- "Most of the benefit can be obtained by beginning screening within 3 years of onset of sexual activity or age 21 (whichever comes first) and screening at least every 3 years"
- "The USPSTF recommends against routinely screening women older than age 65 for cervical cancer if they have had adequate recent screening with normal Pap smears and are not otherwise at high risk for cervical cancer"
- "The USPSTF recommends against routine Pap smear screening in women who have had a total hysterectomy for benign disease"
In additional, clinical practice guidelines address mass screening for cervical cancer by the American College of Obstetricians and Gynecology.[2]. A summary of these guidelines is:[3]
- "Cervical cancer screening should begin at age 21 regardless of age at onset of sexual activity."
- "Cervical cytology screening from age 21 to 29 is recommended every 2 years but should be more frequent in women who are HIV-positive, are immunosuppressed, were exposed in utero to diethylstilbestrol, or have been treated for cervical intraepithelial neoplasia (CIN) 2, 3 or cervical cancer."
- "Women age 30 who have three consecutive negative screens and who do not fit the above criteria for more-frequent screening may be tested every 3 years. Co-testing with cervical cytology and high-risk HPV typing is also appropriate; if both tests are negative, rescreening in 3 years is warranted."
- "Cervical cancer screening is unnecessary in women who have undergone hysterectomies for benign disease and who have no histories of CIN."
- "Discontinuation of screening after age 65 or 70 is reasonable in women with 3 negative consecutive tests and no cervical abnormalities during the previous decade."
- "Women with histories of CIN 2, 3 or cancer should undergo annual screening for 20 years after treatment."
- "HPV vaccination does not change these recommendations."
Accuracy of screening tests
Papanicolaou smear
A systematic review of available studies for detection of cervical intraepithelial neoplasia grade 2 or worse found the follow results.[4]
| ASCUS or worse | High grade or worse | |||
|---|---|---|---|---|
| sensitivity | specificity | sensitivity | specificity | |
| Conventional method | 88% | 71% | 55% | 97% |
| Liquid-based thin prep | 88% | 71% | 57% | 97% |
A more recent study of the conventional method for cervical intraepithelial neoplasia of grade 2 or 3 reported very similar results:[5]
- sensitivity 55%
- specificity 94%
Human papillomavirus testing
- sensitivity 95%[5]
- specificity 97%[5]
Combined testing
If either the Papanicolaou smear or Human papillomavirus testing are abnormal:
- sensitivity 100%[5]
- specificity 93%[5]
Effectiveness of screening
In a randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer "reduces the incidence of grade 2 or 3 cervical intraepithelial neoplasia or cancer detected by subsequent screening examinations."[6]
In another randomized controlled trial, the addition of Human papillomavirus testing to screening for cervical cancer led to earlier detection of CIN3+ lesions.[7]
References
- ↑ Screening for Cervical Cancer, Topic Page. January 2003. U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/clinic/uspstf/uspscerv.htm
- ↑ (2009) Cervical Cytology Screening. The American College of Obstetricians and Gynecology
- ↑ Davis AJ. (2009) Major Changes in ACOG Cervical Cytology Screening Recommendations. Journal Watch Women's Health
- ↑ 4.0 4.1 Arbyn M, Bergeron C, Klinkhamer P, Martin-Hirsch P, Siebers AG, Bulten J (2008). "Liquid Compared With Conventional Cervical Cytology: A Systematic Review and Meta-analysis". Obstet Gynecol 111 (1): 167–177. DOI:10.1097/01.AOG.0000296488.85807.b3. PMID 18165406. Research Blogging.
- ↑ 5.0 5.1 5.2 5.3 5.4 Mayrand MH, Duarte-Franco E, Rodrigues I, et al (2007). "Human papillomavirus DNA versus Papanicolaou screening tests for cervical cancer". N. Engl. J. Med. 357 (16): 1579–88. DOI:10.1056/NEJMoa071430. PMID 17942871. Research Blogging.
- ↑ Naucler P, Ryd W, Törnberg S, et al (2007). "Human papillomavirus and Papanicolaou tests to screen for cervical cancer". N. Engl. J. Med. 357 (16): 1589–97. DOI:10.1056/NEJMoa073204. PMID 17942872. Research Blogging.
- ↑ Bulkmans NW, Berkhof J, Rozendaal L, et al (2007). "Human papillomavirus DNA testing for the detection of cervical intraepithelial neoplasia grade 3 and cancer: 5-year follow-up of a randomised controlled implementation trial". Lancet 370 (9601): 1764–72. DOI:10.1016/S0140-6736(07)61450-0. PMID 17919718. Research Blogging.