Systemic lupus erythematosus
Systemic lupus erythematosis (SLE) is an autoimmune connective tissue disorder. While there is no cure, there have been major advances in its treatment in recent years. There are variants such as drug-induced lupus and discoid lupus.
Initial presentation
Symptoms can be diffuse, but one classical sign, not always present, is a "butterfly-shaped" rash centered on the nose.
Diagnosis
Laboratory tests
A number of immunologic tests are useful in diagnosis, and some in following disease progress. While the "LE prep" microscopic examination of the 1940s is obsolete, the first screening test is the antinuclear antibody titer. When these are elevated, more specific but less sensitive tests come into play, such as anti-double-stranded DNA antibodies (dsDNA) and anti-Smith antibodies (Sm). Antihistone antibodies are elevated in drug-induced lupus. [2]
There may be antibodies to small nuclear ribonucleoproteins, possibly created by cytomegalovirus or Epstein-Barr virus.[3]
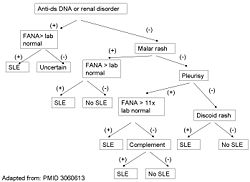
Alternative criteria
Recursive partitioning has been used to identify more parsimonious criteria. [1] This analysis presented two diagnostic classification trees:
1. Simplest classification tree: LSE is diagnosed if the patient has an immunologic disorder (anti-DNA antibodies, anti-Smith antibodies, false positive syphilis test, or LE cells) or malar rash.
- sensitivity = 92%
- specificity = 92%
2. Full classification tree: Uses 6 criteria.
- sensitivity = 97%
- specificity = 95%
Other alternative criteria have been suggested.[4]
Treatment
The beginnings of treatment, in the 1950s, used crude antiinflammatory and immunosuppressants such as ACTH. More refined corticosteroids are the core of therapy, although nonsteroidal anti-inflammatory drugs and antimalarials are used by many rheumatologists. Antimalarials such as hydrochloroquine appear to be immunomodulatory; frank immunosuppressive drugs, especially azathiorine, also are used. [5]
The leading edge of approved treatment, however, are specific monoclonal antibodies.
References
- ↑ 1.0 1.1 Edworthy SM, Zatarain E, McShane DJ, Bloch DA (1988). "Analysis of the 1982 ARA lupus criteria data set by recursive partitioning methodology: new insights into the relative merit of individual criteria". J. Rheumatol. 15 (10): 1493-8. PMID 3060613. [e]
- ↑ Peter H. Schur and Rober H. Scherling (2004), Chapter 5: Laboratory tests in rheumatic disorders, Practical Rheumatology (Third ed.), Mosby, ISBN 03230299396
- ↑ Claudia Azucena Palafox Sánchez et al. (2009), "Reduced IgG anti-small nuclear ribonucleoprotein autoantibody production in systemic lupus erythematosus patients with positive IgM anti-cytomegalovirus antibodies", Arthritis Research & Therapy 11: R27, DOI:10.1186/ar2621
- ↑ Hughes GR (1998). "Is it lupus? The St. Thomas' Hospital "alternative" criteria". Clin. Exp. Rheumatol. 16 (3): 250-2. PMID 9631744. [e]
- ↑ Cynthia Aranow and Ellen M Ginzler (2004), Chapter 45: Connective Tissue Disorders, Systemic Lupus Erythematosis; Treatment of constitutional symptoms, skin, joint, serositis, cardiopulmonar, hematologic and central nervous system manifestations, Practical Rheumatology (Third ed.), Mosby, ISBN 03230299396