Vertebral subluxation: Difference between revisions
imported>Nancy Sculerati MD (Oh, that's how you do it.) |
mNo edit summary |
||
| (53 intermediate revisions by 12 users not shown) | |||
| Line 1: | Line 1: | ||
<font size="1">''This article is about the [[Chiropractic|chiropractic]] concept of vertebral subluxation, for displacement and dislocation of the vertebrae (as described in [[Health science|health science]]) see [[Subluxation of the vertebral joint]].''</font> | {{subpages}} | ||
<font size="1" color="660000">''This article is about the [[Chiropractic|chiropractic]] concept of vertebral subluxation, for displacement and dislocation of the vertebrae (as described in [[Health science|health science]]) see [[Subluxation of the vertebral joint]].''</font> | |||
---- | |||
---- | ---- | ||
[[Image:Spinepixl.jpg|frame|The spine, pelvis and rib cage make up the boney structures that contain, support and protect the vital organ systems that sustain us.]] | [[Image:Spinepixl.jpg|frame|The spine, pelvis and rib cage make up the boney structures that contain, support and protect the vital organ systems that sustain us.]] | ||
'''Vertebral subluxation''' is the term used by chiropractors for the underlying cause of the many signs and symptoms they attribute to misaligned or abnormally functioning spinal vertebrae. A key component of the concept is that subluxated [[vertebra]]e | '''Vertebral subluxation''' is the term used by chiropractors for the underlying cause of the many signs and symptoms they attribute to misaligned or abnormally functioning spinal vertebrae. A key component of the concept is that subluxated [[vertebra]]e must alter the function of the [[Nervous System|nervous system]] and at some point compromise health. The founder of chiropractic, [[D.D. Palmer]], in 1895 suggested that "95% of all diseases were the result of subluxations." Since then, the definition has been altered and refined many times by chiropractors, who use the term to explain why chiropractic may be effective for very diverse conditions. | ||
In 1996, the Association of Chiropractic Colleges, representing all chiropractic colleges in the | In 1996, the Association of Chiropractic Colleges, representing all chiropractic colleges in the United States, unified the definition as "a complex of functional and/or structural and/or pathological articular changes that compromise [[nerve|neural]] integrity and may influence organ system function and general health."<ref>Association of Chiropractic Colleges, [http://www.chirocolleges.org/paradigm_scopet.html Chiropractic Paradigm]</ref> Although the inference that neural integrity is impaired lacks direct evidence, chiropractors nevertheless use it as a model to explain why their treatments seem to have effects on organ systems. | ||
''(For treatment of vertebral subluxation, see [[Spinal adjustment]])'' | ''(For treatment of vertebral subluxation, see [[Spinal adjustment]])'' | ||
==Introduction== | ==Introduction== | ||
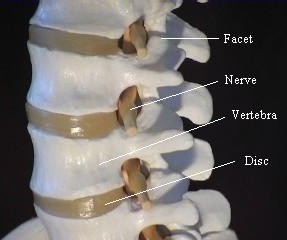
[[Image:Vert1.JPG|100px|right|frame|Model of a motion segment of the spine illustrating the relationship of the vertbrae, disc, facets and nerve.]] | [[Image:Vert1.JPG|100px|right|frame|Model of a motion segment of the spine illustrating the relationship of the vertbrae, disc, facets and nerve with the muscles and ligaments removed.]] | ||
===The human spine=== | ===The human spine=== | ||
The [[human spine]] is comprised of 24 moveable [[vertebra]]e arranged as a column between the [[sacrum]] and the base of the skull. The bony canal formed by the vertebrae surrounds and protects the [[spinal cord]] - the delicate bundle of nerves that is the pathway of communication between the brain and the rest of the body. Each vertebra is connected to the next by three joints - two [[synovial joints]] at the sides (called [[facet joints]]) and a [[intervertebral disk|spongy disc pad]] between the vertebral bodies - as well as by an intricate arrangement of ligaments, muscles and connective tissue. The orientation of these joints, as well as the arrangement of the ligaments and muscles, is ''different for every pair of adjacent vertebrae'', from the neck down to the lowest part of the lumbar spine. Therefore each such pair has a very specific and limited range of movement. Each such uniquely mobile subdivision of the spine, consisting of two adjacent vertebrae and their interconnecting structures, is called a [[spinal motion segment]]. When all these motion segments, from the neck to lumbar spine, are aligned and functioning optimally, the result is a remarkably flexible yet stable bony column which allows a full range of movement, a proper base and support for the rest of the skeleton and muscles, and protection for the spinal cord, allowing the nervous system to convey nerve signals in a way that promotes normal, healthy body function. | The [[human spine]] is comprised of 24 moveable [[vertebra]]e arranged as a column between the [[sacrum]] and the base of the skull. The bony canal formed by the vertebrae surrounds and protects the [[spinal cord]] - the delicate bundle of nerves that is the pathway of communication between the brain and the rest of the body. Each vertebra is connected to the next by three joints - two [[synovial joints]] at the sides (called [[facet joints]]) and a [[intervertebral disk|spongy disc pad]] between the vertebral bodies (a [[syndesmosis|syndesmotic]] joint) - as well as by an intricate arrangement of ligaments, muscles and connective tissue. | ||
The orientation of these joints, as well as the arrangement of the ligaments and muscles, is ''different for every pair of adjacent vertebrae'', from the neck down to the lowest part of the lumbar spine. Therefore each such pair has a very specific and limited range of movement. Each such uniquely mobile subdivision of the spine, consisting of two adjacent vertebrae and their interconnecting structures, is called a [[spinal motion segment]]. When all these motion segments, from the neck to lumbar spine, are aligned and functioning optimally, the result is a remarkably flexible yet stable bony column which allows a full range of movement, a proper base and support for the rest of the skeleton and muscles, and protection for the spinal cord, allowing the nervous system to convey nerve signals in a way that promotes normal, healthy body function. | |||
To enable coordinated movement of all these spinal motion segments, a fine network of nerves innervate the muscles and ligaments that surround the [[joint capsules]], constantly transmitting information to and from the spinal cord, [[cerebellum]] and brain. There are two main classes of these nerves: [[sensory nerves]] that detect the status of the different elements that make up the spine, and [[motor nerves]] that control the function of the muscles of the spine. Some sensory nerves can detect the stretch of ligaments and muscles - information that is used by the spinal cord and higher centers to determine the position and motion of every joint - while others are sensitive to temperature, and can initiate the sensation of [[pain]] from any of the spinal structures which are injured, distorted or lack proper blood supply and nutrition. The posture control centers of the cerebellum integrate the sensory information from the spine and limbs with the requirement for muscle movements needed to execute the whims or wishes of the higher centres of the brain. This enables smooth and coordinated motion, whether voluntary or involuntary, without the mind having to consciously control the contraction of every little muscle. | |||
The motor nerves are thus controlled by the cooperative action of the brain, cerebellum and spinal cord neurons, influenced by the information from the sensory nerves. The contraction of small muscle groups is constantly being changed to best align the spinal column according to minor changes in posture, while the contraction of the larger muscle groups attached to the spine require continuous adjustment to maintain [[balance]]. A second group of motor nerves do not cause skeletal muscle movement as such, but control the [[smooth muscle]] in the walls of [[artery|arteries]], thereby altering local blood flow. Due to the organization of these [[sympathetic nerves|sympathetic]] motor nerves, blood flow in other parts of the body may also be changed, and functions such as [[sweating]] may be affected. A little appreciated function of the nerves that convey impulses from the spine to the tissues ([[efferent nerves]]) is to provide [[growth factors]] that are important for proper cell growth and function in all body tissues. | |||
[[Image:Nadia_Comaneci.jpg|left|frame|The spine can perform significant ranges of motion and shock absorption.]] | [[Image:Nadia_Comaneci.jpg|left|frame|The spine can perform significant ranges of motion and shock absorption.]] | ||
The result of properly functioning spinal motion segments, and a healthy nervous system associated with the spine, is a stable, yet resilient and mobile vertebral column that allows for upright posture and the ability to perform complicated combinations of movement without conscious planning of every detail of the movements. The strength of the athlete and the agility of the gymnast are testaments to the flexibility and durability of the human spine. | The result of properly functioning spinal motion segments, and a healthy nervous system associated with the spine, is a stable, yet resilient and mobile vertebral column that allows for upright posture and the ability to perform complicated combinations of movement without conscious planning of every detail of the movements. The strength of the athlete and the agility of the gymnast are testaments to the flexibility and durability of the human spine. | ||
=== | ===Mechanisms of spinal injury === | ||
As a consequence of a sufficiently forceful spinal injury, vertebral alignment or function can be disturbed permanently. Long term abnormal postural and movement stress on the spine are potentially debilitating. Stresses that can be expected to so affect the spine include the maintenance of fixed improper postures for prolonged periods, chronic repetitive movement patterns, and continuous asymmetrical muscle use - leading to asymmetrical, unbalanced muscle development. At first the spinal changes may be reversible and painless, but if spontaneous resolution does not occur then local muscle spasm, swelling, tenderness, and pain result. | |||
By predominantly unconscious mechanisms, body posture alters to relieve the stress on the spinal structures. This further disturbs the function of the spinal motion segment locally, as well as that of the spine and limbs outside of the original problem area. The initially minor and unheeded changes thus may cause more widely spread injured, inflamed and painful tissue. Damaged tissue may refer pain to other body parts, and damaged nerves can cause dysfunction in organs which they innervate. Thus the person affected by acute or chronic spinal injury can develop complaints such as headache, numbness, or disturbed bowel or bladder function, according to which parts of the spine are injured. In the long term, when abnormal anatomic relationships and movement patterns are not reversed or arrested, the tissues and structures of the spinal motor unit undergo degeneration at an accelerated rate. Such degeneration of the facet joint cartilage and the intervertebral disk complicates the clinical picture with the appearance of the symptoms and signs of osteoarthritis. | |||
====Chiropractic model of disease==== | ====Chiropractic model of disease==== | ||
The | The "Vertebral subluxation model" of disease incorporates this well-accepted account, and goes on to suggest that there are many other important consequences of suboptimal spinal alignment and function. It asserts that, when the information the nerves convey to the brain and spinal cord is disturbed, this affects the organs and tissues that receive a nerve supply from the affected region of the spine. As a result, chiropractors believe that an organ problem is linked to the region of the spine that innervates it. They integrate this information with the other signs and symptoms that were gathered to formulate a rationale for treatment. For instance, they would consider midback pain, tightness between the shoulders and indigestion all to be related to the same condition (See [http://www.chiromatrix.com/Chiropractic_Website_Spine_Simulator/nerve_chart/index.htm this Flash animation] for examples.). They would then treat the ''subluxation'' in the midback in hopes of having an effect on the indigestion. | ||
Thus, while most of the symptoms and health problems attributed to vertebral subluxations are directly related to the musculoskeletal system (the "type M" category), the subluxation theory also says that even tiny changes in position or motion (sometimes too small to be measured by any present objective method) can reduce the body's ability to resist disease, and hence result in conditions of ill health that seem at first sight to be unconnected with the spinal cord. This becomes controversial, as | Thus, while most of the symptoms and health problems attributed to vertebral subluxations are directly related to the musculoskeletal system (the "type M" category), the subluxation theory also says that even tiny changes in position or motion (sometimes too small to be measured by any present objective method) can reduce the body's ability to resist disease, and hence result in conditions of ill health that seem at first sight to be unconnected with the spinal cord. This becomes controversial, as chiropractors are thus always alert to the possibility of a spinal involvement in any disease. | ||
''Subluxation'', ''vertebral subluxation'', and ''vertebral subluxation complex'' (VSC) are concepts used by | ''Subluxation'', ''vertebral subluxation'', and ''vertebral subluxation complex'' (VSC) are concepts used by chiropractors to describe the signs and symptoms that they presume to be effects of alterations in spinal alignment and function. Chiropractors further categorize the process of tissue breakdown into stages of ''subluxation degeneration''. As well as treating conditions that have become symptomatic, chiropractors look for early signs of muscular and postural adaptations as asymmetries in the spine, and try to prevent them from progressing into more serious conditions related to subluxation degeneration. | ||
==Vertebral subluxation complex== | ==Vertebral subluxation complex== | ||
As described by Joseph Flesia DC, the "vertebral subluxation complex" (VSC) has five components | As described by Joseph Flesia DC, the "vertebral subluxation complex" (VSC) has five components: | ||
# ''Spinal kinesiopathology'' — irregularities of the mechanical behavior of the spine | # ''Spinal kinesiopathology'' — irregularities of the mechanical behavior of the spine | ||
| Line 36: | Line 46: | ||
# ''Myopathology'' — muscle spasm, and muscle weakness | # ''Myopathology'' — muscle spasm, and muscle weakness | ||
# ''Histopathology'' — inflammation and tissue swelling, usually around the traumatized area | # ''Histopathology'' — inflammation and tissue swelling, usually around the traumatized area | ||
#''Pathophysiology'' — changes due to the above components usually seen locally as degeneration, fibrous tissue and/or erosion. | #''Pathophysiology'' — changes due to the above components usually seen locally as degeneration, fibrous tissue and/or erosion.<ref>Flesia JM (1992) The vertebral subluxation complex: an integrative perspective. ICA Int Rev Chiropractic (Mar):25-27 [http://chiro.org/LINKS/FULL/The_VSC_1.shtml]</ref> | ||
In the first episode of the VSC, the joint is sprained, and inflammation and swelling appears around it. Uncorrected, a cascade of events can occur: | In the first episode of the VSC, the joint is sprained, and inflammation and swelling appears around it. Uncorrected, a cascade of events can occur: | ||
| Line 46: | Line 56: | ||
*There may also be damage to spinal nerves that carry sensory and motor information to and from the brain, and which are important for the neuromuscular reflexes that control balance and normal movement. | *There may also be damage to spinal nerves that carry sensory and motor information to and from the brain, and which are important for the neuromuscular reflexes that control balance and normal movement. | ||
*With deteriorating spinal function, the neuromuscular habit patterns adapt to the altered spinal biomechanics. In the months after each episode, the motor control | *With deteriorating spinal function, the neuromuscular habit patterns adapt to the altered spinal biomechanics. In the months after each episode, the motor control centers of the nervous system, including those in the cerebellum and spinal cord, "learn" the new abnormal spinal function habit pattern. | ||
Every injury to the spinal cord means that the nervous system must adapt to any consequences of the injury, and compensate for any loss of function. This means that the local spinal reflexes and the motor | Every injury to the spinal cord means that the nervous system must adapt to any consequences of the injury, and compensate for any loss of function. This means that the local spinal reflexes and the motor programs that are controlled by higher brain systems may need to "re-learn" how to execute movements quickly and smoothly. In the brain, such 'motor learning' involves comparing the ''intended'' movement with the ''actual'' movement, and so it depends upon feedback to the brain from proprioceptors and muscle stretch receptors - these are the signals that report to the brain exactly how much muscles have contracted and how a joint has changed its position. The signals are carried by spinal nerves; if their function is impaired, then chiropractors believe that the new motor programs may be built on faulty feedback information, and if so, that they may compensate imperfectly for the injury. With every succeeding injury to the spine, the feedback data become less and less reliable, and the increasingly imperfect motor programs become more likely to incur further injury, creating a downward spiral of spinal function. To change this faulty "learned pattern", chiropractors devise treatment plans that involve spinal adjustments with a specific direction and purpose applied repeatedly over weeks or months, similar to any rehabilitation program designed to re-educate a single injured joint such as a knee. | ||
Chiropractic treatment of the VSC has three major phases. The first phase of | Chiropractic treatment of the VSC has three major phases. The first phase of ''Initial Intensive care'' is to relieve the pain and discomfort and then to stabilize the injured area so the condition will not regress. Often, relief takes several visits and stabilization a few weeks to a few months depending on the age of the patient and the severity of the condition. The second phase is ''Reconstructive/rehabilitative care'', to restore normal function of the spine/body. This includes repair of the soft tissues, spinal joint recovery, muscular rehabilitation, neuromuscular habit pattern recovery, and restoring spinal and whole body homeostasis. Full functional rehabilitation often takes many months or years. If the patient is old and the condition severe, rehabilitative care may be needed indefinitely. The final phase is ''Maintenance care'', to maintain efficient function. | ||
''Initial Intensive care'' is to relieve the pain and discomfort and then to stabilize the injured area so the condition will not regress. Often, relief takes several visits and stabilization a few weeks to a few months depending on the age of the patient and the severity of the condition. The second phase is ''Reconstructive/rehabilitative care'', to restore normal function of the spine/body. This includes repair of the soft tissues, spinal joint recovery, muscular rehabilitation, neuromuscular habit pattern recovery, and restoring spinal and whole body homeostasis. Full functional rehabilitation often takes many months or years. If the patient is old and the condition severe, rehabilitative care may be needed indefinitely. The final phase is ''Maintenance care'', to maintain efficient function. | |||
== Functional theories of vertebral subluxation == | == Functional theories of vertebral subluxation == | ||
The [[Human spine|spinal cord]] contains nerve tracts through which the brain communicates with most of the body. Nerves that branch off the spinal cord form | The [[Human spine|spinal cord]] contains nerve tracts through which the brain communicates with most of the body. Nerves that branch off the spinal cord form "spinal nerve roots" which exit the vertebral column through the openings between adjacent vertebrae (the ''intervertebral foramen''). From here, nerves travel to all parts of the body in a vast communication network that, when working properly, allows the organism to operate in an efficient and well synchronized fashion. Chiropractors think that the structural condition of the spine is critical for ensuring that this nervous communication works properly. V. Strang, D.C., in his book ''Essential Principles of Chiropractic'',<ref>Strang V (1984) ''Essential Principles of Chiropractic'' Davenport : Palmer College of Chiropractic, OCLC: 12102972</ref> suggests several ways by which a misaligned vertebra may interfere with nervous communication. | ||
*''Nerve compression.'' When vertebrae are not properly aligned, the nerve roots and/or spinal cord can become pinched or inflamed. This is the most commonly referenced hypothesis, and perhaps the easiest for patients to understand, but it may be the least likely to occur. | *''Nerve compression.'' When vertebrae are not properly aligned, the nerve roots and/or spinal cord can become pinched or inflamed. This is the most commonly referenced hypothesis, and perhaps the easiest for patients to understand, but it may be the least likely to occur. | ||
*''Proprioceptive insult.'' Neural feedback loops from mechanoreceptors with articular alterations causing hyperactivity of the sensory nerve fibers when the joint structures are under stretch, resulting in a reflex response that tightens the surrounding muscles. | *''Proprioceptive insult.'' Neural feedback loops from mechanoreceptors with articular alterations causing hyperactivity of the sensory nerve fibers when the joint structures are under stretch, resulting in a reflex response that tightens the surrounding muscles. | ||
| Line 62: | Line 71: | ||
*The''Somatopsychic hypothesis'' suggests that subluxation stimulates the ascending paths of the reticular activating system to affect consciousness and feelings of wellbeing. | *The''Somatopsychic hypothesis'' suggests that subluxation stimulates the ascending paths of the reticular activating system to affect consciousness and feelings of wellbeing. | ||
*The ''Neurodystrophic hypothesis'' proposes that tissues whose nerve supply is altered are more susceptible to disease. | *The ''Neurodystrophic hypothesis'' proposes that tissues whose nerve supply is altered are more susceptible to disease. | ||
*''Dentate ligament-cord distortion.'' Upper cervical misalignments might cause the dentate ligaments to put a stress directly on the spinal cord via its attachment to the | *''Dentate ligament-cord distortion.'' Upper cervical misalignments might cause the dentate ligaments to put a stress directly on the spinal cord via its attachment to the "dura mater" (the outer layer of the spinal cord). | ||
*The ''Psychogenic hypothesis'' suggests that emotions such as stress, by causing the skeletal muscles to contract inappropriately, can alter the function of vertebrae. | *The ''Psychogenic hypothesis'' suggests that emotions such as stress, by causing the skeletal muscles to contract inappropriately, can alter the function of vertebrae. | ||
==Scientific studies of the components of the back and spinal column== | ==Scientific studies of the components of the back and spinal column== | ||
The effects of chronic and acute pain, muscle spasm, tissue swelling and degenerative arthritis of the vertebral joints have been investigated extensively, and in many different ways. For example, a research team at the National University of Health Sciences evaluated changes of the lumbar vertebral column after immobilizing vertebrae in laboratory animals to mimic a fixation of the joint.<ref>{{cite journal | author = Cramer G ''et al.'' | title = Degenerative changes following spinal fixation in a small animal model | journal = J Manip Physiol Ther | volume = 27 | pages = 141-54 | year = | id = PMID 15129196}}</ref> This research was of particular interest to | The effects of chronic and acute pain, muscle spasm, tissue swelling and degenerative arthritis of the vertebral joints have been investigated extensively, and in many different ways. For example, a research team at the National University of Health Sciences evaluated changes of the lumbar vertebral column after immobilizing vertebrae in laboratory animals to mimic a fixation of the joint.<ref>{{cite journal | author = Cramer G ''et al.'' | title = Degenerative changes following spinal fixation in a small animal model | journal = J Manip Physiol Ther | volume = 27 | pages = 141-54 | year = | id = PMID 15129196}}</ref> This research was of particular interest to chiropractors because the concept of vertebral subluxation includes the idea of restricted joint mobility as a major cause of problems. The scientists compared the condition of the vertebral body, discs, and facet joints of the experimental group with those of a control group at 2, 4, 6 ,8 and 12 weeks, and found that immobilization of a vertebra resulted in degeneration of the facet joints like that which occurs in osteoarthritis, including [[osteophyte]] formation and cartilage surface changes. | ||
What is more difficult to assess is whether a relatively minor misalignment or functional abnormality that | What is more difficult to assess is whether a relatively minor misalignment or functional abnormality that chiropractors would describe as a subluxation, but which allopathic or osteopathic physicians might consider too minor to be concerned about, can affect an organ system. This is more speculative, and remains relatively untested. It has not been demonstrated that vertebral subluxations contribute to many cases of dysfunction of peripheral organ systems, and it is not clear that spinal manipulations can remedy such a dysfunction even if it has been caused by a pathology of neural control mechanisms.<ref>{{cite journal | author = Davis G, Johns E | title = Renal sympathetic nerve responses to somato-sensory nerve stimulation in normotensive rats | journal = J Auton Nerv Syst | volume = 54 | pages = 59-70 | year = 1995 | id = PMID 7594212}} | ||
<ref>{{cite journal | author = Davis G, Johns E | title = Renal sympathetic nerve responses to somato-sensory nerve stimulation in normotensive rats | journal = J Auton Nerv Syst | volume = 54 | pages = 59-70 | year = 1995 | id = PMID 7594212}} | |||
*{{cite journal | author = Sato A, Swenson R | title = Sympathetic nervous system response to mechanical stress of the spinal column in rats | journal = J Manip Physiol Ther | volume = 7 | pages = 141-7 | year = 1984 | id = PMID 6491548}} | *{{cite journal | author = Sato A, Swenson R | title = Sympathetic nervous system response to mechanical stress of the spinal column in rats | journal = J Manip Physiol Ther | volume = 7 | pages = 141-7 | year = 1984 | id = PMID 6491548}} | ||
*{{cite journal | author = Davis G, Johns E | title = Effect of somatic nerve stimulation on the kidney in intact, vagotomized and carotid sinus-denervated rats | journal = J Physiol | volume = 432 | pages = 573-84 | year = | id = PMID 1886069}} | *{{cite journal | author = Davis G, Johns E | title = Effect of somatic nerve stimulation on the kidney in intact, vagotomized and carotid sinus-denervated rats | journal = J Physiol | volume = 432 | pages = 573-84 | year = | id = PMID 1886069}} | ||
| Line 76: | Line 84: | ||
==History== | ==History== | ||
<BLOCKQUOTE> | |||
In its chiropractic context, the term 'subluxation' was first described by | "When any of the vertebrae become displaced or too prominent, the patient experiences inconvenience from a local derangement in the nerves of the part. He, in consequence, is tormented with a train of nervous symptoms, which are as obscure in their origin as they are stubborn in their nature..." - Edward Harrison MD (1759-1838)<ref>*{{cite journal | author = Kent C | title = Models of Vertebral Subluxation | journal = J Ventral Sublux Res | volume = 1| pages = 1-7 | year = 1996 }} [http://www.jvsr.com/archives/kent.pdf] (Accessed 2007-02-04) quotes this from an article by Terrett AJC (1987) The search for the subluxation: an investigation of medical literature to 1985. Chiro Hist 7:29</ref> | ||
</BLOCKQUOTE> | |||
The original investigation and early research into this entity are shrouded in confusion, due to lack of formal notes, and the political struggle that ensued to establish a stable 'fountainhead' for the entire chiropractic profession. A popular version was that Palmer restored long-lost hearing to a janitor by realigning bones of his spine. Chiropractic treatments gained notoriety during the 1918 | In its chiropractic context, the term ''subluxation'' was first described by D.D. Palmer, who developed the chiropractic system in the late 1800's. Palmer's understanding, based on the scientific knowledge of the time, was that a disturbance of nerve supplies to tissues and organs could explain the changes produced after correction ("adjustments") of misaligned spinal bones, and he believed that he had discovered the cause of the vast majority of all diseases suffered by mankind. | ||
<BLOCKQUOTE> | |||
"Physiologists divide nerve-fibers, which form the nerves, into two classes, afferent and efferent. Impressions are made on the peripheral afferent fiber-endings; these create sensations which are transmitted to the center of the nervous system. Efferent nerve-fibers carry impulses out from the center to their endings. Most of these go to muscles and are therefore called motor impulses; some are secretory and enter glands; a portion are inhibitory their function being to restrain secretion. Thus, nerves carry impulses outward and sensations inward. The activity of these nerves, or rather their fibers, may become excited or allayed by impingement, the result being a modification of functionating - too much or not enough action - which is disease."<ref name="SciArtPhi">Palmer DD (1910) ''The Science, Art and Philosophy of Chiropractic'' Portland, Oregon: Portland Printing House Company p20</ref> | |||
</BLOCKQUOTE> | |||
The original investigation and early research into this entity are shrouded in confusion, due to lack of formal notes, and the political struggle that ensued to establish a stable 'fountainhead' for the entire chiropractic profession. A popular version was that Palmer restored long-lost hearing to a janitor by realigning bones of his spine. Chiropractic treatments gained notoriety during the 1918 "Spanish Flu" epidemic, when it was claimed that patients receiving adjustments had significant less mortality than those treated with conventional medical treatments. | |||
The early chiropractors used palpation and the anatomy of the nervous system as a guide. They created the vitalistic term [[Innate Intelligence]] to explain the apparently metaphysical brain and body interactions that they observed, suggesting that subluxations blocked these interactions. In seeking to be more specific in their interventions, they seized enthusiastically on the newly-discovered [[X-ray]] technology, and introduced an early heat-sensing device (the neurocalometer) to help in diagnosing subluxations. In those early years, the medical establishment criticized chiropractic, saying that the conditions that early chiropractors treated were only [[Psychosomatic illness|psychophysiological disorders]]. In response, [[B. J. Palmer]] (the son of Daniel Palmer) opened a research clinic as part of the Palmer College of Chiropratic. Patients who entered the clinic were first examined by | The early chiropractors used palpation and the anatomy of the nervous system as a guide. They created the vitalistic term [[Innate Intelligence]] to explain the apparently metaphysical brain and body interactions that they observed, suggesting that subluxations blocked these interactions. In seeking to be more specific in their interventions, they seized enthusiastically on the newly-discovered [[X-ray]] technology, and introduced an early heat-sensing device (the neurocalometer) to help in diagnosing subluxations. In those early years, the medical establishment criticized chiropractic, saying that the conditions that early chiropractors treated were only [[Psychosomatic illness|psychophysiological disorders]]. In response, [[B. J. Palmer]] (the son of Daniel Palmer) opened a research clinic as part of the Palmer College of Chiropratic. Patients who entered the clinic were first examined by a medical doctor, who made a diagnosis. They were then sent to the chiropractic part of the clinic, treated, and sent back to the medical doctor for evaluation. Since then, chiropractors have sought a deeper understanding of the mechanisms and effects of the vertebral subluxation. Today, they often use motion X-rays, surface EMG, and digital thermography. | ||
== Critiques == | == Critiques == | ||
An area of debate among chiropractors is whether | (See also [[Critical views of chiropractic]]) | ||
An area of debate among chiropractors is whether the concept of vertebral subluxation is 'metaphysical' (standing for a disorder the exact nature of which is not understood, as posited by B.J. Palmer) or 'literal' (implying a specific mechanical disorder). Furthermore, conventional physical therapists, MDs and osteopathic physicians attach a very different meaning to the term ''subluxation'' than chiropractors do; they only refer to a body part as "having a subluxation" if it can be ''objectively'' demonstrated that it is out of its functional position (''See [[Subluxation of the vertebral joint]]''). Thus, when a radiologist reads a spinal x-ray as "showing subluxation of a vertebra", he or she always means that a bone in the spinal column is ''visibly'' displaced; for example, a pediatrician calls the elbow joint of a child "subluxed" in the condition '[[Nursemaid's elbow]]' only if the lower arm bones are pulled out of the joint capsule and the child cannot move the forearm. A chiropractor, on the other hand, may diagnose a subluxation ''subjectively'', by manual palpation - he or she will apply specific pressure to one joint in isolation, and if it does not move or have an "elastic feel" like those above and below it, a "subluxation" will be diagnosed. The subjective nature of such diagnoses, and whether such subtle changes are functionally significant if they exist at all, as well as chiropractic's different use of the term "subluxation", are at the heart of much controversy over chiropractic. | |||
The concept of vertebral subluxation has been plagued with problems since its inception. Some chiropractors, such as Christopher Kent <ref>{{cite journal | author = Kent C | title = Models of vertebral subluxation | journal = J Ventral Sublux Res | volume = 1| pages = 1-7 | year = 1996 }} [http://www.jvsr.com/archives/kent.pdf]</ref> argue that attempts to tie vertebral subluxation to a precise definition are misconceived, arguing that it is an intellectual construct used to explain the success of the chiropractic adjustment. They argue that similar abstract entities are used in many branches of science. For example, at various times, "genes", "gravity", "the ego" and "the mind" have all been similar heuristic devices, "useful fictions" used to provisionally explain phenomena that exceeded then-current understanding. By this argument, chiropractors say it is incorrect to say that chiropractic is based on the theory that vertebral subluxations "cause pinched nerves that cause disease"; rather, it is based on the empirical evidence of therapeutic benefits of spinal adjustment, and the theory of vertebral subluxation is a proposed explanation of why it works. Others, like Ronald Carter, Past President of the Canadian Chiropractic Association have argued strongly that the chiropractic profession should eliminate the concept of vertebral subluxation and adopt a model of chiropractic more consistent with other health professions, arguing that the concept is an unnecessary impediment to integration with other professions.<ref>[http://www.jcca-online.org/client/cca/JCCA.nsf/objects/Commentary:+Subluxation-the+silent+killer/$file/2-commentary.pdf Subluxation - The Silent Killer]</ref> | |||
In a 2005 article on vertebral subluxation, Keating and colleagues argue that "there is nothing inherently dogmatic or anti-scientific in the notion that an articular lesion may have health consequences, or that correction of joint dysfunction may relieve symptoms and/or improve health."<ref name="subluxation_dogma">**{{cite journal | author = Keating JC ''et al.'' | title = Subluxation: dogma or science? | journal = Chiropr Osteopat | volume = 13| pages = 17 | year = 2005 }} Published online 2005 August 10. DOI 10.1186/1746-1340-13-17. [http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1208927 Accessed 2007-02-07].</ref> They argue that the current inability to predict the effects of a subluxation and the benefits of correcting it, does not make this hypothetical construct valueless, and that "it would be just as inappropriate to dispose of this largely untested theory without data as it is to proclaim its meaningfulness without adequate evidence." Quoting [[Carl Sagan]]'s dictum that "extraordinary claims require extraordinary evidence", they suggest that | In a 2005 article on vertebral subluxation, the historian of chiropractic Joseph Keating and colleagues argue that "there is nothing inherently dogmatic or anti-scientific in the notion that an articular lesion may have health consequences, or that correction of joint dysfunction may relieve symptoms and/or improve health."<ref name="subluxation_dogma">**{{cite journal | author = Keating JC ''et al.'' | title = Subluxation: dogma or science? | journal = Chiropr Osteopat | volume = 13| pages = 17 | year = 2005 }} Published online 2005 August 10. DOI 10.1186/1746-1340-13-17. [http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1208927 Accessed 2007-02-07].</ref> They argue that the current inability to predict the effects of a subluxation and the benefits of correcting it, does not make this hypothetical construct valueless, and that "it would be just as inappropriate to dispose of this largely untested theory without data as it is to proclaim its meaningfulness without adequate evidence." Quoting [[Carl Sagan]]'s dictum that "extraordinary claims require extraordinary evidence", they suggest that chiropractors should avoid unreasonable speculation and presentation of theory as fact. In their summary they state: | ||
<BLOCKQUOTE> | |||
"The dogma of subluxation is perhaps the greatest single barrier to professional development for chiropractors. It skews the practice of the art in directions that bring ridicule from the scientific community and uncertainty among the public. Failure to challenge subluxation dogma perpetuates a marketing tradition that inevitably prompts charges of quackery. Subluxation dogma leads to legal and political strategies that may amount to a house of cards and warp the profession's sense of self and of mission. Commitment to this dogma undermines the motivation for scientific investigation of subluxation as hypothesis, and so perpetuates the cycle."<ref name="subluxation_dogma"/> | |||
</BLOCKQUOTE> | |||
== References == | == References == | ||
<references/> | <references/> | ||
[[Category:Articles to be assessed for citability]] | |||
[[Category:Suggestion Bot Tag]] | |||
[[Category: | |||
Latest revision as of 17:01, 4 November 2024
This article is about the chiropractic concept of vertebral subluxation, for displacement and dislocation of the vertebrae (as described in health science) see Subluxation of the vertebral joint.
Vertebral subluxation is the term used by chiropractors for the underlying cause of the many signs and symptoms they attribute to misaligned or abnormally functioning spinal vertebrae. A key component of the concept is that subluxated vertebrae must alter the function of the nervous system and at some point compromise health. The founder of chiropractic, D.D. Palmer, in 1895 suggested that "95% of all diseases were the result of subluxations." Since then, the definition has been altered and refined many times by chiropractors, who use the term to explain why chiropractic may be effective for very diverse conditions.
In 1996, the Association of Chiropractic Colleges, representing all chiropractic colleges in the United States, unified the definition as "a complex of functional and/or structural and/or pathological articular changes that compromise neural integrity and may influence organ system function and general health."[1] Although the inference that neural integrity is impaired lacks direct evidence, chiropractors nevertheless use it as a model to explain why their treatments seem to have effects on organ systems.
(For treatment of vertebral subluxation, see Spinal adjustment)
Introduction
The human spine
The human spine is comprised of 24 moveable vertebrae arranged as a column between the sacrum and the base of the skull. The bony canal formed by the vertebrae surrounds and protects the spinal cord - the delicate bundle of nerves that is the pathway of communication between the brain and the rest of the body. Each vertebra is connected to the next by three joints - two synovial joints at the sides (called facet joints) and a spongy disc pad between the vertebral bodies (a syndesmotic joint) - as well as by an intricate arrangement of ligaments, muscles and connective tissue.
The orientation of these joints, as well as the arrangement of the ligaments and muscles, is different for every pair of adjacent vertebrae, from the neck down to the lowest part of the lumbar spine. Therefore each such pair has a very specific and limited range of movement. Each such uniquely mobile subdivision of the spine, consisting of two adjacent vertebrae and their interconnecting structures, is called a spinal motion segment. When all these motion segments, from the neck to lumbar spine, are aligned and functioning optimally, the result is a remarkably flexible yet stable bony column which allows a full range of movement, a proper base and support for the rest of the skeleton and muscles, and protection for the spinal cord, allowing the nervous system to convey nerve signals in a way that promotes normal, healthy body function.
To enable coordinated movement of all these spinal motion segments, a fine network of nerves innervate the muscles and ligaments that surround the joint capsules, constantly transmitting information to and from the spinal cord, cerebellum and brain. There are two main classes of these nerves: sensory nerves that detect the status of the different elements that make up the spine, and motor nerves that control the function of the muscles of the spine. Some sensory nerves can detect the stretch of ligaments and muscles - information that is used by the spinal cord and higher centers to determine the position and motion of every joint - while others are sensitive to temperature, and can initiate the sensation of pain from any of the spinal structures which are injured, distorted or lack proper blood supply and nutrition. The posture control centers of the cerebellum integrate the sensory information from the spine and limbs with the requirement for muscle movements needed to execute the whims or wishes of the higher centres of the brain. This enables smooth and coordinated motion, whether voluntary or involuntary, without the mind having to consciously control the contraction of every little muscle.
The motor nerves are thus controlled by the cooperative action of the brain, cerebellum and spinal cord neurons, influenced by the information from the sensory nerves. The contraction of small muscle groups is constantly being changed to best align the spinal column according to minor changes in posture, while the contraction of the larger muscle groups attached to the spine require continuous adjustment to maintain balance. A second group of motor nerves do not cause skeletal muscle movement as such, but control the smooth muscle in the walls of arteries, thereby altering local blood flow. Due to the organization of these sympathetic motor nerves, blood flow in other parts of the body may also be changed, and functions such as sweating may be affected. A little appreciated function of the nerves that convey impulses from the spine to the tissues (efferent nerves) is to provide growth factors that are important for proper cell growth and function in all body tissues.
The result of properly functioning spinal motion segments, and a healthy nervous system associated with the spine, is a stable, yet resilient and mobile vertebral column that allows for upright posture and the ability to perform complicated combinations of movement without conscious planning of every detail of the movements. The strength of the athlete and the agility of the gymnast are testaments to the flexibility and durability of the human spine.
Mechanisms of spinal injury
As a consequence of a sufficiently forceful spinal injury, vertebral alignment or function can be disturbed permanently. Long term abnormal postural and movement stress on the spine are potentially debilitating. Stresses that can be expected to so affect the spine include the maintenance of fixed improper postures for prolonged periods, chronic repetitive movement patterns, and continuous asymmetrical muscle use - leading to asymmetrical, unbalanced muscle development. At first the spinal changes may be reversible and painless, but if spontaneous resolution does not occur then local muscle spasm, swelling, tenderness, and pain result.
By predominantly unconscious mechanisms, body posture alters to relieve the stress on the spinal structures. This further disturbs the function of the spinal motion segment locally, as well as that of the spine and limbs outside of the original problem area. The initially minor and unheeded changes thus may cause more widely spread injured, inflamed and painful tissue. Damaged tissue may refer pain to other body parts, and damaged nerves can cause dysfunction in organs which they innervate. Thus the person affected by acute or chronic spinal injury can develop complaints such as headache, numbness, or disturbed bowel or bladder function, according to which parts of the spine are injured. In the long term, when abnormal anatomic relationships and movement patterns are not reversed or arrested, the tissues and structures of the spinal motor unit undergo degeneration at an accelerated rate. Such degeneration of the facet joint cartilage and the intervertebral disk complicates the clinical picture with the appearance of the symptoms and signs of osteoarthritis.
Chiropractic model of disease
The "Vertebral subluxation model" of disease incorporates this well-accepted account, and goes on to suggest that there are many other important consequences of suboptimal spinal alignment and function. It asserts that, when the information the nerves convey to the brain and spinal cord is disturbed, this affects the organs and tissues that receive a nerve supply from the affected region of the spine. As a result, chiropractors believe that an organ problem is linked to the region of the spine that innervates it. They integrate this information with the other signs and symptoms that were gathered to formulate a rationale for treatment. For instance, they would consider midback pain, tightness between the shoulders and indigestion all to be related to the same condition (See this Flash animation for examples.). They would then treat the subluxation in the midback in hopes of having an effect on the indigestion.
Thus, while most of the symptoms and health problems attributed to vertebral subluxations are directly related to the musculoskeletal system (the "type M" category), the subluxation theory also says that even tiny changes in position or motion (sometimes too small to be measured by any present objective method) can reduce the body's ability to resist disease, and hence result in conditions of ill health that seem at first sight to be unconnected with the spinal cord. This becomes controversial, as chiropractors are thus always alert to the possibility of a spinal involvement in any disease.
Subluxation, vertebral subluxation, and vertebral subluxation complex (VSC) are concepts used by chiropractors to describe the signs and symptoms that they presume to be effects of alterations in spinal alignment and function. Chiropractors further categorize the process of tissue breakdown into stages of subluxation degeneration. As well as treating conditions that have become symptomatic, chiropractors look for early signs of muscular and postural adaptations as asymmetries in the spine, and try to prevent them from progressing into more serious conditions related to subluxation degeneration.
Vertebral subluxation complex
As described by Joseph Flesia DC, the "vertebral subluxation complex" (VSC) has five components:
- Spinal kinesiopathology — irregularities of the mechanical behavior of the spine
- Neuropathophysiology/neuropathology — compressed or facilitated nerve tissue
- Myopathology — muscle spasm, and muscle weakness
- Histopathology — inflammation and tissue swelling, usually around the traumatized area
- Pathophysiology — changes due to the above components usually seen locally as degeneration, fibrous tissue and/or erosion.[2]
In the first episode of the VSC, the joint is sprained, and inflammation and swelling appears around it. Uncorrected, a cascade of events can occur:
- At first, the sprained joint is hypermobile, but as it heals it can become fixated (hypomobility). This may be accompanied by fibrosis that, in time, results in degeneration and remodeling (a fibrotic/calcific enlargement of the joint that is at first visible only on MRI studies, but which later can be seen by X-ray imaging). Compensation and adaptation can occur, and the problems may extend to the joint above and sometimes to the joint below, to which the biomechanics of the spine must adapt. With repeated episodes of the VSC, the spine accumulates more and more of these problem sites, resulting in deteriorating spinal function or "abnormal orthopedic functional programs".
- Muscle dysfunction (myopathology) also occurs immediately, and can lead to long-term spasm or to muscle weakness and atrophy. This can cause the spine to acquire abnormal, habitual, and harmful positions and movement patterns, described as muscle "sets".
- There may also be damage to spinal nerves that carry sensory and motor information to and from the brain, and which are important for the neuromuscular reflexes that control balance and normal movement.
- With deteriorating spinal function, the neuromuscular habit patterns adapt to the altered spinal biomechanics. In the months after each episode, the motor control centers of the nervous system, including those in the cerebellum and spinal cord, "learn" the new abnormal spinal function habit pattern.
Every injury to the spinal cord means that the nervous system must adapt to any consequences of the injury, and compensate for any loss of function. This means that the local spinal reflexes and the motor programs that are controlled by higher brain systems may need to "re-learn" how to execute movements quickly and smoothly. In the brain, such 'motor learning' involves comparing the intended movement with the actual movement, and so it depends upon feedback to the brain from proprioceptors and muscle stretch receptors - these are the signals that report to the brain exactly how much muscles have contracted and how a joint has changed its position. The signals are carried by spinal nerves; if their function is impaired, then chiropractors believe that the new motor programs may be built on faulty feedback information, and if so, that they may compensate imperfectly for the injury. With every succeeding injury to the spine, the feedback data become less and less reliable, and the increasingly imperfect motor programs become more likely to incur further injury, creating a downward spiral of spinal function. To change this faulty "learned pattern", chiropractors devise treatment plans that involve spinal adjustments with a specific direction and purpose applied repeatedly over weeks or months, similar to any rehabilitation program designed to re-educate a single injured joint such as a knee.
Chiropractic treatment of the VSC has three major phases. The first phase of Initial Intensive care is to relieve the pain and discomfort and then to stabilize the injured area so the condition will not regress. Often, relief takes several visits and stabilization a few weeks to a few months depending on the age of the patient and the severity of the condition. The second phase is Reconstructive/rehabilitative care, to restore normal function of the spine/body. This includes repair of the soft tissues, spinal joint recovery, muscular rehabilitation, neuromuscular habit pattern recovery, and restoring spinal and whole body homeostasis. Full functional rehabilitation often takes many months or years. If the patient is old and the condition severe, rehabilitative care may be needed indefinitely. The final phase is Maintenance care, to maintain efficient function.
Functional theories of vertebral subluxation
The spinal cord contains nerve tracts through which the brain communicates with most of the body. Nerves that branch off the spinal cord form "spinal nerve roots" which exit the vertebral column through the openings between adjacent vertebrae (the intervertebral foramen). From here, nerves travel to all parts of the body in a vast communication network that, when working properly, allows the organism to operate in an efficient and well synchronized fashion. Chiropractors think that the structural condition of the spine is critical for ensuring that this nervous communication works properly. V. Strang, D.C., in his book Essential Principles of Chiropractic,[3] suggests several ways by which a misaligned vertebra may interfere with nervous communication.
- Nerve compression. When vertebrae are not properly aligned, the nerve roots and/or spinal cord can become pinched or inflamed. This is the most commonly referenced hypothesis, and perhaps the easiest for patients to understand, but it may be the least likely to occur.
- Proprioceptive insult. Neural feedback loops from mechanoreceptors with articular alterations causing hyperactivity of the sensory nerve fibers when the joint structures are under stretch, resulting in a reflex response that tightens the surrounding muscles.
- Somatosympathetic reflexes Organ functions can be reflexly affected by stimulation of skin or muscle, thereby affecting , for example, heart rate and blood pressure.
- Somatosomatic reflexes Stimulation of the skin and muscle in one area of the body can result in reflex activity in muscles of other parts of the body.
- Viscerosomatic reflexes Afferent fibers from organs (the viscera) can trigger reflex muscle and skin reactions that cause pain and tightened muscles, and which might result in vertebral subluxations.
- TheSomatopsychic hypothesis suggests that subluxation stimulates the ascending paths of the reticular activating system to affect consciousness and feelings of wellbeing.
- The Neurodystrophic hypothesis proposes that tissues whose nerve supply is altered are more susceptible to disease.
- Dentate ligament-cord distortion. Upper cervical misalignments might cause the dentate ligaments to put a stress directly on the spinal cord via its attachment to the "dura mater" (the outer layer of the spinal cord).
- The Psychogenic hypothesis suggests that emotions such as stress, by causing the skeletal muscles to contract inappropriately, can alter the function of vertebrae.
Scientific studies of the components of the back and spinal column
The effects of chronic and acute pain, muscle spasm, tissue swelling and degenerative arthritis of the vertebral joints have been investigated extensively, and in many different ways. For example, a research team at the National University of Health Sciences evaluated changes of the lumbar vertebral column after immobilizing vertebrae in laboratory animals to mimic a fixation of the joint.[4] This research was of particular interest to chiropractors because the concept of vertebral subluxation includes the idea of restricted joint mobility as a major cause of problems. The scientists compared the condition of the vertebral body, discs, and facet joints of the experimental group with those of a control group at 2, 4, 6 ,8 and 12 weeks, and found that immobilization of a vertebra resulted in degeneration of the facet joints like that which occurs in osteoarthritis, including osteophyte formation and cartilage surface changes.
What is more difficult to assess is whether a relatively minor misalignment or functional abnormality that chiropractors would describe as a subluxation, but which allopathic or osteopathic physicians might consider too minor to be concerned about, can affect an organ system. This is more speculative, and remains relatively untested. It has not been demonstrated that vertebral subluxations contribute to many cases of dysfunction of peripheral organ systems, and it is not clear that spinal manipulations can remedy such a dysfunction even if it has been caused by a pathology of neural control mechanisms.[5]
History
"When any of the vertebrae become displaced or too prominent, the patient experiences inconvenience from a local derangement in the nerves of the part. He, in consequence, is tormented with a train of nervous symptoms, which are as obscure in their origin as they are stubborn in their nature..." - Edward Harrison MD (1759-1838)[6]
In its chiropractic context, the term subluxation was first described by D.D. Palmer, who developed the chiropractic system in the late 1800's. Palmer's understanding, based on the scientific knowledge of the time, was that a disturbance of nerve supplies to tissues and organs could explain the changes produced after correction ("adjustments") of misaligned spinal bones, and he believed that he had discovered the cause of the vast majority of all diseases suffered by mankind.
"Physiologists divide nerve-fibers, which form the nerves, into two classes, afferent and efferent. Impressions are made on the peripheral afferent fiber-endings; these create sensations which are transmitted to the center of the nervous system. Efferent nerve-fibers carry impulses out from the center to their endings. Most of these go to muscles and are therefore called motor impulses; some are secretory and enter glands; a portion are inhibitory their function being to restrain secretion. Thus, nerves carry impulses outward and sensations inward. The activity of these nerves, or rather their fibers, may become excited or allayed by impingement, the result being a modification of functionating - too much or not enough action - which is disease."[7]
The original investigation and early research into this entity are shrouded in confusion, due to lack of formal notes, and the political struggle that ensued to establish a stable 'fountainhead' for the entire chiropractic profession. A popular version was that Palmer restored long-lost hearing to a janitor by realigning bones of his spine. Chiropractic treatments gained notoriety during the 1918 "Spanish Flu" epidemic, when it was claimed that patients receiving adjustments had significant less mortality than those treated with conventional medical treatments.
The early chiropractors used palpation and the anatomy of the nervous system as a guide. They created the vitalistic term Innate Intelligence to explain the apparently metaphysical brain and body interactions that they observed, suggesting that subluxations blocked these interactions. In seeking to be more specific in their interventions, they seized enthusiastically on the newly-discovered X-ray technology, and introduced an early heat-sensing device (the neurocalometer) to help in diagnosing subluxations. In those early years, the medical establishment criticized chiropractic, saying that the conditions that early chiropractors treated were only psychophysiological disorders. In response, B. J. Palmer (the son of Daniel Palmer) opened a research clinic as part of the Palmer College of Chiropratic. Patients who entered the clinic were first examined by a medical doctor, who made a diagnosis. They were then sent to the chiropractic part of the clinic, treated, and sent back to the medical doctor for evaluation. Since then, chiropractors have sought a deeper understanding of the mechanisms and effects of the vertebral subluxation. Today, they often use motion X-rays, surface EMG, and digital thermography.
Critiques
(See also Critical views of chiropractic)
An area of debate among chiropractors is whether the concept of vertebral subluxation is 'metaphysical' (standing for a disorder the exact nature of which is not understood, as posited by B.J. Palmer) or 'literal' (implying a specific mechanical disorder). Furthermore, conventional physical therapists, MDs and osteopathic physicians attach a very different meaning to the term subluxation than chiropractors do; they only refer to a body part as "having a subluxation" if it can be objectively demonstrated that it is out of its functional position (See Subluxation of the vertebral joint). Thus, when a radiologist reads a spinal x-ray as "showing subluxation of a vertebra", he or she always means that a bone in the spinal column is visibly displaced; for example, a pediatrician calls the elbow joint of a child "subluxed" in the condition 'Nursemaid's elbow' only if the lower arm bones are pulled out of the joint capsule and the child cannot move the forearm. A chiropractor, on the other hand, may diagnose a subluxation subjectively, by manual palpation - he or she will apply specific pressure to one joint in isolation, and if it does not move or have an "elastic feel" like those above and below it, a "subluxation" will be diagnosed. The subjective nature of such diagnoses, and whether such subtle changes are functionally significant if they exist at all, as well as chiropractic's different use of the term "subluxation", are at the heart of much controversy over chiropractic.
The concept of vertebral subluxation has been plagued with problems since its inception. Some chiropractors, such as Christopher Kent [8] argue that attempts to tie vertebral subluxation to a precise definition are misconceived, arguing that it is an intellectual construct used to explain the success of the chiropractic adjustment. They argue that similar abstract entities are used in many branches of science. For example, at various times, "genes", "gravity", "the ego" and "the mind" have all been similar heuristic devices, "useful fictions" used to provisionally explain phenomena that exceeded then-current understanding. By this argument, chiropractors say it is incorrect to say that chiropractic is based on the theory that vertebral subluxations "cause pinched nerves that cause disease"; rather, it is based on the empirical evidence of therapeutic benefits of spinal adjustment, and the theory of vertebral subluxation is a proposed explanation of why it works. Others, like Ronald Carter, Past President of the Canadian Chiropractic Association have argued strongly that the chiropractic profession should eliminate the concept of vertebral subluxation and adopt a model of chiropractic more consistent with other health professions, arguing that the concept is an unnecessary impediment to integration with other professions.[9]
In a 2005 article on vertebral subluxation, the historian of chiropractic Joseph Keating and colleagues argue that "there is nothing inherently dogmatic or anti-scientific in the notion that an articular lesion may have health consequences, or that correction of joint dysfunction may relieve symptoms and/or improve health."[10] They argue that the current inability to predict the effects of a subluxation and the benefits of correcting it, does not make this hypothetical construct valueless, and that "it would be just as inappropriate to dispose of this largely untested theory without data as it is to proclaim its meaningfulness without adequate evidence." Quoting Carl Sagan's dictum that "extraordinary claims require extraordinary evidence", they suggest that chiropractors should avoid unreasonable speculation and presentation of theory as fact. In their summary they state:
"The dogma of subluxation is perhaps the greatest single barrier to professional development for chiropractors. It skews the practice of the art in directions that bring ridicule from the scientific community and uncertainty among the public. Failure to challenge subluxation dogma perpetuates a marketing tradition that inevitably prompts charges of quackery. Subluxation dogma leads to legal and political strategies that may amount to a house of cards and warp the profession's sense of self and of mission. Commitment to this dogma undermines the motivation for scientific investigation of subluxation as hypothesis, and so perpetuates the cycle."[10]
References
- ↑ Association of Chiropractic Colleges, Chiropractic Paradigm
- ↑ Flesia JM (1992) The vertebral subluxation complex: an integrative perspective. ICA Int Rev Chiropractic (Mar):25-27 [1]
- ↑ Strang V (1984) Essential Principles of Chiropractic Davenport : Palmer College of Chiropractic, OCLC: 12102972
- ↑ Cramer G et al.. "Degenerative changes following spinal fixation in a small animal model". J Manip Physiol Ther 27: 141-54. PMID 15129196.
- ↑ Davis G, Johns E (1995). "Renal sympathetic nerve responses to somato-sensory nerve stimulation in normotensive rats". J Auton Nerv Syst 54: 59-70. PMID 7594212.
- Sato A, Swenson R (1984). "Sympathetic nervous system response to mechanical stress of the spinal column in rats". J Manip Physiol Ther 7: 141-7. PMID 6491548.
- Davis G, Johns E. "Effect of somatic nerve stimulation on the kidney in intact, vagotomized and carotid sinus-denervated rats". J Physiol 432: 573-84. PMID 1886069.
- Bolton P (2000). "Reflex effects of vertebral subluxations: the peripheral nervous system. An update". J Manip Physiol Ther 23: 101-3. PMID 10714535.
- Budgell B (2000). "Reflex effects of subluxation: the autonomic nervous system". J Manip Physiol Ther 23: 104-6. PMID 10714536.
- ↑ *Kent C (1996). "Models of Vertebral Subluxation". J Ventral Sublux Res 1: 1-7. [2] (Accessed 2007-02-04) quotes this from an article by Terrett AJC (1987) The search for the subluxation: an investigation of medical literature to 1985. Chiro Hist 7:29
- ↑ Palmer DD (1910) The Science, Art and Philosophy of Chiropractic Portland, Oregon: Portland Printing House Company p20
- ↑ Kent C (1996). "Models of vertebral subluxation". J Ventral Sublux Res 1: 1-7. [3]
- ↑ Subluxation - The Silent Killer
- ↑ 10.0 10.1 **Keating JC et al. (2005). "Subluxation: dogma or science?". Chiropr Osteopat 13: 17. Published online 2005 August 10. DOI 10.1186/1746-1340-13-17. Accessed 2007-02-07.